As a long time Crohn’s patient, I am often sought out for advice on handling the disease by newly diagnosed patients and their families. And while awareness of Crohn’s is much greater than it was twenty years ago, most people really don’t understand much about the disease or the way it impacts a patient’s life. so I’ve decided to write a four-part document that hopefully explains to new Crohn’s patients and the general public what to expect and how to cope. these posts cover the medical symptoms tips for patients living with the disease and tips for people who know someone living with Crohn’s.
In this post, I’ll cover symptoms.
Crohn’s Disease is, without a doubt, one of the more debilitating medical conditions around right now. For those unfamiliar with it, Crohn’s is an auto-immune disorder that affects the digestive tract. Symptoms include weight loss, frequent (and often uncontrollable) bowel movements, diarrhea, nausea, bloating, intestinal discomfort and pain (which can mimic appendicitis) and fatigue. Symptoms also include the typical aches, pains and fevers usually associated with the flu. Because it is an auto-immune disease, people with Crohn’s often find themselves later developing other auto-immune disorders – for instance, I have rheumatoid arthritis and developed hay fever about 7 years ago. I’ve met other patients who developed even more severe types of auto-immune disorders, such as lupus.
Very little is really understood about Crohn’s. nobody knows why it occurs – there seems to be a genetic factor (an extra gene is found in about 90% of Crohn’s patients), but nothing has been completely ruled out. Ethnicity, diet and activities all may be related – or maybe not. likewise, there isn’t a cure. what has advanced since I was first diagnosed 20 years ago is understanding how the disease functions and causes other functions of the body to stop. that has led to better treatment options and generally, a better quality of life for those of us affected. once, the disease was thought more prevalent in women than men, but the rates of affliction, once adjusted for populations, are actually about the same. Almost every ethnic group is affected, although peoples of Asian and African descent have lower incidence rates than Caucasians.
Odds are if you’re a new patient, then you are in the 16-25 year old range: this is when about 80% of new cases are first diagnosed. (I was 6 weeks shy of my 26th birthday when first diagnosed). that being said, new cases are diagnosed in every age group. since I’ve no personal experience with pediatric Crohn’s, I won’t pretend to offer advice for anyone looking for information about Crohn’s and young children.
Symptomatically, Crohn’s is similar to Ulcerative Colitis. The similarities often confuse a person only cursorily aware of both conditions, which often leads to them confusing the two. I’ve had past co-workers and current friends often assume that because Crohn’s and UC are related and so similar symptomatically, that they are the same. but when I’ve had severe flare-ups of the disease, they are often shocked when they come visit and find me hooked up to dozens of tubes and wires, all needed to keep me alive and stable.
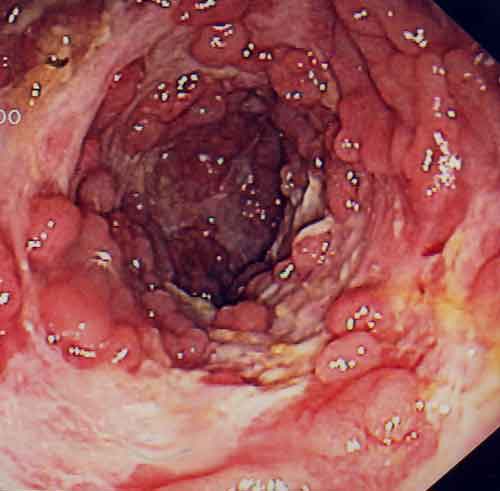
The symptoms are where the similarities end. both cause ulcerations (inflamed areas) to appear in the colon, but the ones from Crohn’s disease burrow deeper into the tissue and can appear anywhere in the digestive tract. In my particular case, the upper palate, gums, a section of the small intestine called the duodenum and another called the ileum are affected in addition to two spots in my large intestine and another in my colon. Another big difference: in severe cases of colitis, a type of surgery called an ostomy can be performed, curing the disease (although at a high price). For some severe cases of Crohn’s usually where the tissue is badly damaged), surgery is also done – but removing the affected areas doesn’t cure the disease. It will reappear in another area of the GI tract.
Since Crohn’s patients generally have difficulty digesting food, it isn’t uncommon to find them malnourished even when relatively symptom free (by the way, those of us in the Crohn’s community generally refer to these periods as being in remission). Unfortunately, the type of malnutrition can vary from patient to patient. The reason is because so many different parts of the digestive tract are affected and each part is responsible for processing different nutrients. regardless, the malnutrition is a major contributor to all types of related problems. since each part of the body relies on the digestive system to function properly, people with Crohn’s often suffer from other system breakdowns. Their hair, skin and nails can become dry and brittle; they may suffer anemia, dehydration, high blood pressure, osteoporosis – the list includes virtually every other organ in the body. Add in the side-effects from long-term use of some of the more common medications used to treat Crohn’s, and the results can be even more system breakdowns. For example, the use of Mesalamine drugs can lead to excessive (and particularly foul smelling gas). as for myself, repeated exposure to very high doses of corticosteroids has resulted in cataracts and osteopenia (the precursor to osteoporosis). The calcium deficiency from my Crohn’s along a Crohn’s inflammation in my upper palate and the drug cocktail I’m on, resulted in my losing all of my teeth before I was 30 (although, my dentures look damn good!).