 By Lia Steakley
By Lia Steakley
New research published in the Journal of Clinical Oncology shows that decreases in depression among women with advanced breast cancer are associated with improved survival rates for these patients.
In the 14-year long study (subscription required), researchers had 125 women complete surveys measuring symptoms of depression at the beginning of the study and at four-month intervals for the initial year. All participants were given educational materials, and half also participated in 90-minute group sessions led by co-therapy teams. Results showed patients with improving depressive symptoms had significantly longer median survival times than those with worsening symptoms: 53.6 months compared to 25.1 months.
In the following Q&A, Stanford psychiatrist David Spiegel, MD, who was principal investigator on the study, discusses the significance of the results, the physiological connection between depression and breast cancer, and why it’s worthwhile for breast cancer patients to be screened for depression.
What are the implications of these findings?
Depression is a risk factor for shorter breast cancer survival time, just as it is associated with poorer prognosis with heart disease. this means that identifying and treating depression in cancer patients is an important part of good medical management of breast cancer. Depression is treatable, both with medication and psychotherapy. it is not simply a reaction to cancer, but rather a complicating co-morbid illness that occurs in some but not all cancer patients.
What is the physiological connection between depression and breast cancer survival?
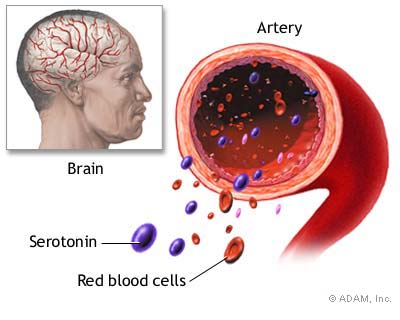
Depression is associated with abnormalities in the stress hormone cortisol, which mobilizes glucose into the blood to prepare us to ‘fight or flee.’ Depressed people often have higher than normal cortisol levels, and they tend to lose the variation on cortisol normally seen throughout the day and night. Normal cortisol levels are four times as high in the morning as they are in the evening. Loss of this diurnal pattern also predicts shorter survival with breast cancer, a finding we published (.pdf) in the Journal of the National Cancer Institute a decade ago. Cortisol can inhibit the function of tumor suppressor genes, such as BrCA1. it is also potently immunosuppressive, and our immune systems help us to control the growth of tumors with specialized cells called natural killer (NK) cells, and others. Depression also inhibits health-related behavior, ranging from getting normal sleep and exercise to adhering with medical treatment. Depressed people are often socially avoidance, and may not get the social support they need. so in many ways, depression can worsen outcome with breast cancer.
In light of these findings, would it be worthwhile for physicians to consider screening breast cancer patients for depression?
yes, it is a complicating co-morbid condition, not a normal reaction to having cancer. Screening and aggressive treatment will improve quality of life and may well extend survival.