Atherosclerosis, the buildup of fatty deposits on the walls of major arteries, can kill without warning. the disease causes few symptoms in its early stages, so sufferers are often hit with a heart attack or stroke before they realize anything is wrong. now researchers have devised a way to spot the deposits before they cause serious harm by using a combination of infrared light and ultrasound.
To detect atherosclerosis early, doctors need to spot fat inside artery walls. They can glean some information by bombarding soft tissue (anything that’s not bone) with infrared radiation from a laser, which passes through the tissue until it hits a specific chemical bond, causing it to vibrate like a spring. different chemical bonds absorb infrared radiation of different wavelengths, so the radiation absorbed by a tissue sample can give doctors some clue to what’s inside it. But to diagnose atherosclerosis, doctors not only need to know that tissue contains fat but also need to see that it’s on the inside of an artery wall.
In the new study, researchers took advantage of the fact that infrared-induced vibration of chemical bonds is swiftly damped by surrounding tissue; the energy is converted to heat. this leads to rapid expansion of the tissue, which sends a pressure wave traveling outward in all directions to the surface of the sample, where it is emitted as ultrasound. by using a series of detectors to pick up the ultrasound, the team realized that it could work out where the expansion took place—a technique called photoacoustic imaging.
“We are not the first to use photoacoustic imaging,” explains biomedical engineer Ji-Xin Cheng of Purdue University in West Lafayette, Indiana. (In the past, the absorption of visible light by hemoglobin has been used to image blood flow around skin cancer.) “But it wasn’t clear that molecular vibration could be detected in this way. we believe this opens a very new direction for the field.”
The researchers tested their idea by imaging arteries removed from slaughtered pigs that had had varying degrees of atherosclerosis. They bombarded the samples with infrared radiation at a wavelength particularly likely to be absorbed by the carbon-hydrogen bonds in the deadly fatty deposits lining atherosclerotic arteries. by measuring the ultrasound emission from the irradiated tissue, the researchers created detailed images of the deposits in a completely noninvasive way with minimal interference from the surrounding tissue.
The team’s experiments, reported this month in Physical Review Letters, suggest that the technique could probe about 7 millimeters into the body. That would allow doctors to see into the walls of blood vessels or to visualize fat in muscle under the skin.
Biophysicist Sunney Xie of Harvard University is impressed by the potential of the new technique. “A penetration depth of the order of a few millimeters is certainly good for surgeons,” he says. Xie also suggests the technique could be used during surgery to locate lesions precisely and to check that they have been removed completely.
Systems biologist Matthias Nahrendorf of Harvard Medical School in Boston, an expert in atherosclerosis imaging, agrees that the technique is scientifically impressive. But he says it needs further work before it can make a meaningful difference to the diagnosis of atherosclerosis: “It’s an impressive piece of engineering and physics that’s fairly far from clinical translation and not a game-changing advance over what is out there.”
Nahrendorf estimates that, unless the researchers can increase penetration depth to more than 10 centimeters, it will still be necessary to insert catheters into arteries to investigate possible atherosclerosis—a major procedure that is usually performed only if a patient has shown prior symptoms of atherosclerosis such as shortness of breath or chest pains.
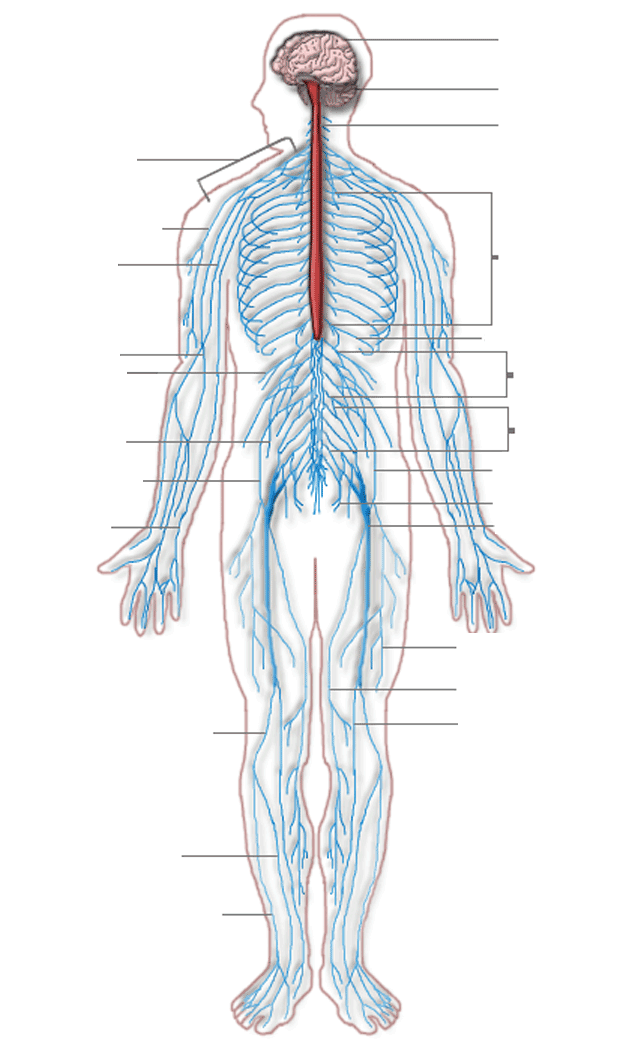
Cheng is excited by the possibilities of the new technique beyond atherosclerosis screening. by choosing different infrared wavelengths, he says, researchers can excite different bonds and study a variety of processes in soft tissue, such as scar formation and the changes to the central nervous system that occur in diseases such as Alzheimer’s and multiple sclerosis. “I think the applications of this are very broad, and we are working on these applications now.”