Upon my arrival to Kitale, I promised myself that one of the places I did not want to visit was the local hospital.
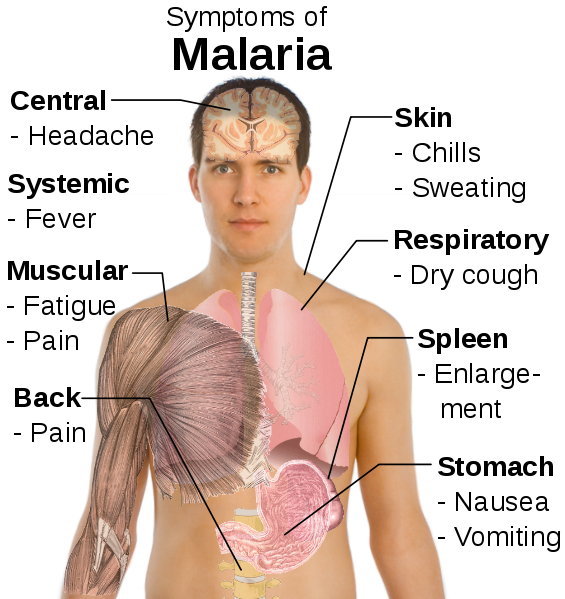
I woke up last week Friday, feeling extraordinarily weak. not, I need to rest kind of “weak.” More like the entire energy had been drained out of me, kind of “weak.” this was after a long, long restless night. My joints ache. I feel cold, even shivering, in 23 degree Celsius weather. My entire body feels uncomfortable, like an alien suit sewn underneath my skin. My head hurts. a few hours later, I tread slowly, uphill, in the sun (I sound like someone’s grandfather now, don’t I?) to the hospital, confident that I had Malaria. After a long wait, blood test, and another long wait, the result is in: Typhoid Fever.
During the first injection, I literally felt better at the point of injection. until the vomiting-inducing effect of the injection kicked in. as I hadn’t eaten for over a day, I ended up wreathing for a blissful two-minutes over a metal sink. My stomach is twisting in knots, like an aggressive, gargantuan maid wringing a wet shirt dry. a kind nurse pats my back, before delivering the second injection. Sweet.
The entire point of this story though, is less about my experience, and more about some of the challenges Malaria poses in the developing world – two primarily. One is detection. due to the similarities in symptoms between Malaria and other diseases, such as Typhoid, patients of Malaria are diagnosed with Typhoid, or vice versa. the result is naturally improper treatment. (I hope that I am not in this category!)
The second challenge is largely a result of the first: over-medication. In areas where equipment is often lacking to properly diagnose Malaria, patients with Malaria-like symptoms, that may well be a very bad flu, are given Malaria medication. the result is that individuals, in increasingly large amounts, are becoming resistant to conventional forms of Malaria treatment, without any subsequent increase in preventative protection from the disease.
These are over and above the traditional challenges that individuals with low-incomes face in accessing treatment to quality medical care. the total cost for my medicine was $10 USD. That can be the entire monthly salary of an entry-level role at a Kenyan corporation for a University educated student. for an uneducated mother of two who is a micro-entrepreneur, the resources for this treatment maybe entirely unavailable.
I fear the only effect this post may have is encouraging awareness. Outside of highlighting the important of a functional government in providing sustainable and affordable access to health care, there are few other recommendations I can provide.
While the role of the Bill and Melinda Gates Foundation, in addition to the Clinton Foundation, are commendable in addressing diseases like Malaria, the sustainability, efficacy and reach of these approaches remains to be seen.