Battery-powered hot pants could be a new way to tackle a common symptom of prostate disease. The fabric boxer shorts, designed to be worn underneath underpants, have small, self-heating elements in the material.
They are being used in a clinical trial to treat urinary hesitancy and retention — conditions which affect men of all ages and make it difficult for them to pass water.
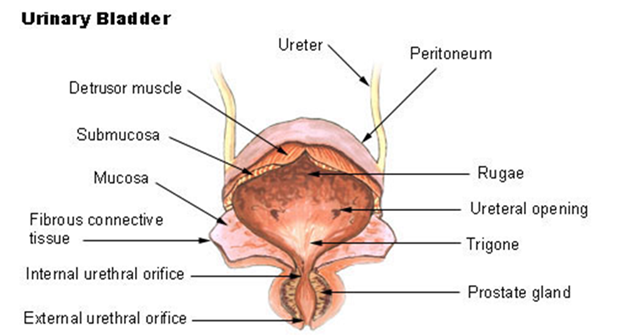
Urine retention is particularly common in men with an enlarged prostate gland as it blocks the exit to the bladder, causing symptoms such as difficulty starting urination, a frequent need to go to the loo, and difficulty emptying the bladder fully.
Battery-powered hot pants are being used in a clinical trial to treat urinary hesitancy and retention – conditions which affect men of all ages
These symptoms can range from mild to severe and in some cases can mean a complete inability to urinate. The condition is usually treated with medication or surgery.
The new hot pants, developed by U.S. firm ThermaRx and on trial at the Mobley Clinical Research Centre, Houston, Texas, are designed to produce low-level heat to improve symptoms.
The idea of using a warm garment is based on anecdotal evidence and case reports suggesting that some urinary problems can be effectively reduced by external skin heating — what’s known as the hot-tub Jacuzzi effect.
The theory is that the warmth of the pants relaxes muscle cells in the bladder neck, urinary sphincter and pelvic floor.
Doctors also believe that heat somehow reduces impulses from part of the body’s communication network, called the autonomic nervous system.
This network is largely independent of voluntary control and regulates many basic functions such as bladder contraction. For some reason, that medics say is unclear, this system contributes to the problems caused by prostate enlargement by preventing the bladder from emptying.
It’s estimated that 60 per cent of men aged 60 or over have some degree of prostate enlargement, also known as benign prostatic hyperplasia (BPH).
The exact cause is unknown, but research suggests hormones probably play an important role. some studies show a hormone called dihydrotestosterone (DHT), which increases levels with age, may stimulate the growth of the prostate.
The prostate, a small gland found only in men, is located in the pelvis, between the penis and bladder, and surrounds the urethra, the tube that carries urine.
In the trial of 60 men with BPH and urinary retention symptoms, participants will be given a drink and then the pants switched on.
The pants take five to 15 minutes to have a warming effect. Ultrasound-based measurements of bladder volume will be taken before and after urination, and one of the measurements will be to see if the use of the device improves bladder emptying.
Researchers say the same idea could also work for nocturia, the need to urinate several times during the night.
Raj Persad, consultant urological surgeon and a senior clinical lecturer at the University of Bristol, who was not involved in the research, said: ‘It sounds like a reasonable non-invasive technique to try out and the results could be interesting in the early phases of obstruction due to BPH — especially for people who cannot tolerate or do not want tablets.
‘Medically, our understanding of the autonomic nervous system is poor, but there are clearly influences on bladder and bowel function from it.’
He adds: ‘one only has to think how many times one feels the need to visit the bathroom before a stressful event, such as sitting exams, or how the cold weather can increase the need for the loo. These are both autonomic effects.
‘Presumably, this technology somehow affects or modulates the autonomic nervous systems impulses to the bladder.’
A common prostate condition may be successfully treated with pollen extract.
A new placebo-controlled trial of 60 patients with prostatitis, an inflammatory condition of the prostate gland that will affect half of men at some time in their lives, found that two out of three men improved when given the treatment.
The study, at Sinai Medical Centre in California, focused on non-bacterial prostatitis, where the patient has the signs and symptoms of prostate inflammation, but no evidence of bacterial infection.
Symptoms can include severe pelvic pain. Painkillers and warm baths are usually recommended to ease symptoms of non-bacterial prostatitis.
The trial patients were given pollen tablets three times a day for six months.
The scientists are unclear how the therapy works, but previous studies suggest the pollen can trigger anti-inflammatory effects in the body.