WASHINGTON, D.C.—Parasites get a bad rap for a good reason. they cause a litany of diseases with a terrifying host of symptoms. but mounting evidence suggests that they can also prevent disease. And now there’s genetic evidence to suggest that’s true. new research presented here yesterday at the annual meeting of the American Association for the Advancement of Science (which publishes ScienceNOW) finds that a gene associated with increased risk of asthma is also linked to resistance against a parasitic worm.
Scientists have long suspected that allergies and asthma—common in the developed world and relatively rare in poor countries—are the result of lack of exposure to microbes. this 2-decade-old idea, called the hygiene hypothesis, suggests that lack of exposure to dangerous parasites in childhood makes the adaptive arm of the immune system more likely to overreact when it comes into contact with benign allergens.
Kathleen Barnes, an anthropologist and genetics expert at Johns Hopkins University in Baltimore, Maryland, and her colleagues have been studying the relationship between asthma and one particular parasitic worm, Schistosoma mansoni, in Conde, a cluster of rural fishing villages on the coast of Brazil. the worm is common in the region, and up to 85% of residents are exposed to it.
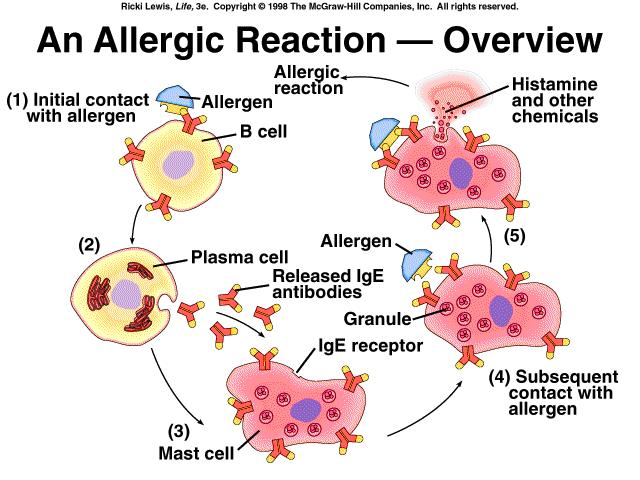
Previous studies have shown that, in areas like Conde, where parasitic worms are endemic, individuals who produce the most worm-specific antibodies—in particular, an antibody called IgE, which triggers inflammation—tend to be the most resistant to worm infection. According to Barnes’s research, that resistance appears to be about 30% heritable.
The researchers noted that after they administered medication to rid Conde’s residents of worms, the incidence of asthma and allergy symptoms increased. So Barnes hypothesized that the mutations that help individuals fend off parasitic worms might be the same mutations that make them susceptible to asthma and allergies. if an individual produces a lot of IgE in response to a worm, he or she might also produce a lot of IgE in response to an allergen.
The team collected blood and stool samples from 850 people in Conde. they tested their blood for antibodies to the worm to gauge their immune response and searched their stool for worm eggs to determine how heavily they were infected. the researchers decided to focus on genes that have been linked to asthma risk. they were particularly interested in IL-33, a gene linked to inflammation that is overexpressed in the lung tissue of asthmatics compared with people without the disease. “IL-33 stands as one of the strongest candidate genes for asthma to date,” Barnes says.
Barnes and colleagues selected 23 genetic markers throughout the gene and tested whether any of them were associated with worm resistance in the residents of Conde. five of them did show a strong association, and those happened to be the exact same markers that are associated with asthma. “And what we’re most excited about is that the relationship is inverse,” Barnes says. “So a [gene variant] that conferred risk to asthma confers protection against [worm infection].”
The researchers posit that natural selection might favor mutations that protect against worm infection and that those same mutations might inadvertently increase the risk of other diseases, such as asthma. the researchers haven’t yet found the exact mutation responsible for the worm resistance and asthma susceptibility. to find that, they’ll have to “drill down deeper,” Barnes says. She speculates that the culprit may be a mutation located in a genome region that regulates activity of the IL-33 gene.
Jennifer Ingram, a cell biologist who studies asthma at Duke University in Durham, North Carolina, says the finding that deworming medication increased the incidence of asthma symptoms is “striking.” She adds that Barnes’s work is important because it points the field toward molecular mechanisms that might contribute to asthma.
David Van Sickle, a medical anthropologist at the University of Wisconsin, Madison, who presented during the same session as Barnes, points out that the global prevalence estimates for asthma are based largely on asking people whether a physician has ever told them they have asthma. but diagnoses vary from culture to culture. Van Sickle found, for example, that physicians in India are much less likely than doctors in Wisconsin to diagnose a person who has clear symptoms of asthma with the disease. So the true prevalence of asthma in India or other countries could be higher or lower than current estimates. Changes in the prevalence of asthma wouldn’t necessarily nullify the hygiene hypothesis, he says, but they could complicate the picture. still, he says Barnes’s work is “elegant.”
Follow our full coverage of AAAS 2011