Abstract Full Text (PDF) Alert me when this article is cited Alert me if a correction is posted Citation Map Email this article to a Colleague Similar articles in this journal Similar articles in PubMed Alert me to new issues of the journal Add to my Articles & Searches Download to citation manager Citing Articles via HighWire Citing Articles via Google Scholar Articles by Addington, J. Articles by Addington, D. Search for Related Content PubMed Citation Articles by Addington, J. Articles by Addington, D. am J Psychiatry 155:974-975, July 1998 Copyright 1998 American Psychiatric Association brief Report Smoking Cessation Treatment for Patients with Schizophrenia Jean Addington, Ph.D., Nady el-Guebaly, M.D., William Campbell, M.D., David C. Hodgins, Ph.D., and Donald Addington, M.D.
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES OBJECTIVE: this study was an uncontrolled trial to assess the efficacy of a smoking cessation group program modified for individuals with schizophrenia. METHOD: Fifty outpatients with schizophrenia were divided into five groups who met separately for seven weekly sessions of a smoking cessation program. The subjects’ schizophrenic and extrapyramidal symptoms were assessed before the group sessions began and after they had been completed. Assessments of smoking were made at those times and at 3-month and 6-month follow-ups. RESULTS: Forty-two percent of the subjects had stopped smoking at the end of the group sessions; 16% remained abstinent at 3 months, and 12% at 6 months. These changes were statistically significant. there was no change in the positive or negative symptoms of schizophrenia. CONCLUSIONS: The results suggest that it is possible for individuals with schizophrenia to stop smoking. (Am J Psychiatry 1998; 155:974–976)
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES Individuals with schizophrenia smoke more than the general population and other psychiatric diagnostic groups (1, 2). in addition to the associated health hazards, the use of nicotine may interfere with the benefits of antipsychotic medication and increase side effects (2–4). Despite the increased focus on the health hazards of smoking, there are few reports of interventions for patients with schizophrenia (5, 6). A recent study (7) suggested that schizophrenic patients are interested in stopping smoking and are as motivated to do so as other people are. unfortunately, the symptoms and cognitive and social deficits associated with schizophrenia make participation in existing smoking cessation programs difficult. Thus, the purpose of this study was to evaluate the effectiveness of a smoking cessation program modified for persons with schizophrenia.
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES The inclusion criteria for the study were that subjects be aged 18–65 years, be regular smokers, be stable outpatients, and meet the DSM-IV criteria for schizophrenia or schizoaffective disorder on the basis of a chart review. Persons who met the DSM-IV criteria for substance abuse or dependence (other than nicotine) were excluded. Sixty-five outpatients referred themselves to the study and completed the initial assessments. Fifteen had dropped out by the second group session.
Fifty subjects (29 male and 21 female) completed the group program and all four assessments. their mean age was 40 years (SD=8), they had a mean of 12 years (SD=2) of education, and their mean number of previous hospital admissions was eight (SD=9). The majority were single, lived alone, and received government financial support. Twenty-eight subjects were taking typical antipsychotics, and 22 were taking atypical antipsychotics. The mean dose in chlorpromazine equivalents was 425.50 mg/day (range=20–1350). this was a relatively naive group of quitters: 30 subjects had made no previous attempt to quit, 17 had used nicotine replacement, and three had attended a smoking cessation program.
Two raters were trained on all measures, and adequate reliability was maintained. The Positive and Negative Syndrome Scale (8) and the Simpson-Angus Rating Scale for extrapyramidal effects (9) were administered before and after the group program. Two other scales were used at all assessments: the Fagerstrom Test for Nicotine Dependence (10) and the Reasons for Quitting Scale (11), a 20-item self-report scale that assesses four dimensions of motivation to quit smoking, namely, health concerns, self-control, immediate reinforcement, and social influence. at each assessment subjects were classified as smoking or abstinent at that point. Reports of abstinence were validated biochemically by determination of urinary cotinine levels. Cotinine has a half-life of 14 days, has been used to validate self-reports of not having smoked in the past 7 days, and may be useful up to 3–4 weeks for validation (12).
The subjects were given a complete description of the study, after which written informed consent was obtained. Assessments occurred before the group sessions began, after the group sessions ended, and 3 and 6 months after the last group session. The subjects were divided into five separate groups (N=12 for two; N=10, N=9, and N=7 for the other three) for the seven weekly group sessions, which lasted for 75 minutes. All sessions were led by a psychiatric nurse experienced in working with schizophrenic patients and in groups. she became a certified facilitator for smoking cessation by participating in a 1.5-day training workshop sponsored by the Alberta Lung Association. The cotherapist was a graduate student. The group treatment was based on the seven-session group program “Freedom From Smoking” designed by the American Lung Association and was modified to meet the needs of individuals with schizophrenia. Adherence to the modified program was monitored throughout and ranged from 94% to 98% for each of the seven sessions.
The group program included positive reinforcement, learning and practicing alternative behaviors, and anxiety reduction strategies. there was a tolerance for positive symptoms, and social and financial limitations were considered. Teaching modifications were made to address neurocognitive deficits such as restricted information-processing capacity, memory and attentional difficulties, and poor executive functioning. A manual describing this group program in more detail is available from the first author.
Nicotine patches were offered to all subjects in conjunction with group attendance. Dosing began at 21 mg/day for 6 weeks and was then tapered to 14 mg/day and 7 mg/day for 2 weeks each.
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES All reported results are for the 50 subjects who completed the group program. at the beginning of the program, the subjects were smoking an average of 28 cigarettes per day (SD=12) and had been smoking for an average of 23 years (SD=9). Nicotine dependence was high; the mean score was 6.39 (SD=2.09). Forty subjects initially used the nicotine patch. The average number of sessions attended was six; 50% of the subjects attended all seven sessions. According to the Reasons for Quitting Scale, the subjects were consistently more intrinsically than extrinsically motivated. their degree of motivation did not differ from that reported in the literature for nonpsychiatric subjects (7, 11). in order of importance, reasons for quitting were health concerns, self-control, immediate reinforcement, and social influence. changes over time were not significant.
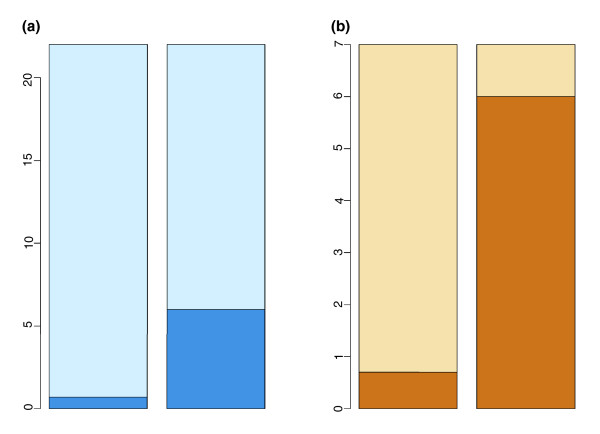
Paired t tests revealed no changes in schizophrenic and extrapyramidal symptoms from before the group sessions to after (table 1). McNemar tests indicated that a significant number of the subjects (N=21) had quit smoking at the end of the group program. although this number decreased at both the 3-month and 6-month follow-ups, the numbers were still significantly different from the pregroup assessment (table 1). All but one of the subjects who quit had used the nicotine patch.
View this table:[in this window][in a new window]
we divided the subjects into four groups—those who never stopped smoking and those who were abstinent at the end of the group program, at 3-month follow-up, and at 6-month follow-up—and conducted analyses of variance to determine variables that might differentiate the groups. The results demonstrated no differences among any of the groups in medications, demographic characteristics, smoking variables, symptoms, or motivation. The one exception was attendance at the group sessions: the subjects who remained abstinent at the 3- and 6-month follow-ups attended all seven group sessions, those who had quit smoking at the end of the group program had attended 6.5 group sessions, and those who did not quit attended an average of 5.5 sessions (F=6.12, df=3,46, p=0.001).
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES Lack of a control group limits this study. however, the results were generally promising. These individuals had a long history of schizophrenia and had been heavy smokers for many years. All of the subjects expressed a strong desire to stop smoking, were intrinsically motivated, and generally showed good attendance. A substantial proportion of the subjects (42%) stopped smoking for at least 4 weeks. this number decreased to 16% at 3 months and to 12% at 6 months. although these percentages are less than the 20%–25% rates for quitting in the general population (13), they are comparable to the 15% rate at 6 months reported by Ziedonis et al. (6). These results suggest that it is possible for individuals with schizophrenia to stop smoking; the difficult part is maintaining abstinence. Quitting smoking should not be considered an impossible task for individuals suffering from schizophrenia. A group approach with nicotine replacement and with modifications of the group sessions could be effective.
Presented at the 150th annual meeting of the American Psychiatric Association, San Diego, may 17–22, 1997. Received June 20, 1997; revisions received Oct. 10, 1997, and Jan. 20, 1998; accepted Jan. 30, 1998. From the Department of Psychiatry, University of Calgary. Address reprint requests to Dr. Jean Addington, Department of Psychiatry, Foothills Hospital, 1403 29th St., N.W., Calgary, Alta., Canada T2N 2T9; jmadding{at}acs.ucalgary.ca (e-mail). Supported by a grant from the National Health, Research and Development Program of Canada.
TOP ABSTRACT INTRODUCTION METHOD RESULTS DISCUSSION REFERENCES
This article has been cited by other articles:
T. L Purvis, S. E Mambourg, T. M Balvanz, H. E Magallon, and R. H PhamSafety and Effectiveness of Varenicline in a Veteran Population with a High Prevalence of Mental Illness Ann. Pharmacother., may 1, 2009; 43(5): 862 – 867.[Abstract] [Full Text] [PDF] N. E. Morden, L. A. Mistler, W. B. Weeks, and S. J. BartelsHealth Care for Patients with Serious Mental Illness: Family Medicine’s Role J am Board Fam Med, March 1, 2009; 22(2): 187 – 195.[Abstract] [Full Text] [PDF] C. D. Morris, G. J. Tedeschi, J. A. Waxmonsky, M. may, and A. A. GieseTobacco Quitlines and Persons with Mental Illnesses: Perspective, Practice, and Direction Journal of the American Psychiatric Nurses Association, February 1, 2009; 15(1): 32 – 40.[Abstract] [PDF] T. V. Cooper, B. S. Hanson, R. S. Burke, and Y. M. HuntSequential Treatment for Nicotine Dependence and Postcessation Weight Concern in a Female Diagnosed with Paranoid Schizophrenia Clinical Case Studies, August 1, 2008; 7(4): 340 – 355.[Abstract] [PDF] A. Baker, R. Richmond, M. Haile, T. J. Lewin, V. J. Carr, R. L. Taylor, S. Jansons, and K. WilhelmA Randomized Controlled Trial of a Smoking Cessation Intervention Among People with a Psychotic Disorder am J Psychiatry, November 1, 2006; 163(11): 1934 – 1942.[Abstract] [Full Text] [PDF] M. McFall, A. J. Saxon, C. E. Thompson, D. Yoshimoto, C. Malte, K. Straits-Troster, E. Kanter, X.-H. A. Zhou, C. M. Dougherty, and B. SteeleImproving the Rates of Quitting Smoking for Veterans with Posttraumatic Stress Disorder am J Psychiatry, July 1, 2005; 162(7): 1311 – 1319.[Abstract] [Full Text] [PDF] K. A. Sacco, A. Termine, A. Seyal, M. M. Dudas, J. C. Vessicchio, S. Krishnan-Sarin, P. I. Jatlow, B. E. Wexler, and T. P. GeorgeEffects of Cigarette Smoking on Spatial Working Memory and Attentional Deficits in Schizophrenia: Involvement of Nicotinic Receptor Mechanisms Arch Gen Psychiatry, June 1, 2005; 62(6): 649 – 659.[Abstract] [Full Text] [PDF] W. J. O’Donnell, R. L. Kradin, A. E. Evins, and C. WittramCase 39-2004 – A 52-Year-Old Woman with Recurrent Episodes of Atypical Pneumonia N. Engl. J. Med., December 23, 2004; 351(26): 2741 – 2749.[Full Text] [PDF] A. R. Lingford-Hughes, S. Welch, and D. J. NuttEvidence-Based Guidelines for the Pharmacological Management of Substance Misuse, Addiction and Comorbidity: Recommendations from the British Association for Psychopharmacology J Psychopharmacol, September 1, 2004; 18(3): 293 – 335.[PDF] I. Kagan, R. Kigli-Shemesh, N. Tabak, M. Z Abramowitz, and J. MargolinPatient Rights and Law: tobacco smoking in psychiatric wards and the Israeli Prevention of Smoking Act Nursing Ethics, September 1, 2004; 11(5): 472 – 478.[Abstract] [PDF] I. Cormac, D. Martin, and M. FerriterImproving the physical health of long-stay psychiatric in-patients Adv. Psychiatr. Treat., March 1, 2004; 10(2): 107 – 115.[Abstract] [Full Text] [PDF] O. Freudenreich and T. A. SternClinical Experience with the Management of Schizophrenia in the General Hospital Psychosomatics, February 1, 2003; 44(1): 12 – 23.[Abstract] [Full Text] [PDF] B. Spring, R. Pingitore, and D. E. McChargueReward Value of Cigarette Smoking for Comparably Heavy Smoking Schizophrenic, Depressed, and Nonpatient Smokers am J Psychiatry, February 1, 2003; 160(2): 316 – 322.[Abstract] [Full Text] [PDF] N. el-Guebaly, J. Cathcart, S. Currie, D. Brown, and S. GlosterSmoking Cessation Approaches for Persons with Mental Illness or Addictive Disorders Psychiatr Serv, September 1, 2002; 53(9): 1166 – 1170. [Abstract] [Full Text] [PDF] E. Weiner, M. P. Ball, A. Summerfelt, J. Gold, and R. W. BuchananEffects of Sustained-Release Bupropion and Supportive Group Therapy on Cigarette Consumption in Patients with Schizophrenia am J Psychiatry, April 1, 2001; 158(4): 635 – 637.[Abstract] [Full Text] M. Phelan, L. Stradins, and S. MorrisonPhysical health of people with severe mental illness BMJ, February 24, 2001; 322(7284): 443 – 444.[Full Text] A. Lucksted, L. B. Dixon, and J. B. SemblyA Focus Group Pilot Study of Tobacco Smoking Among Psychosocial Rehabilitation Clients Psychiatr Serv, December 1, 2000; 51(12): 1544 – 1548. [Abstract] [Full Text] [PDF] K. Lasser, J. W. Boyd, S. Woolhandler, D. U. Himmelstein, D. McCormick, and D. H. BorSmoking and Mental Illness: A Population-Based Prevalence Study JAMA, November 22, 2000; 284(20): 2606 – 2610.[Abstract] [Full Text] [PDF] T. P. George, D. M. Ziedonis, A. Feingold, W. T. Pepper, C. A. Satterburg, J. Winkel, B. J. Rounsaville, and T. R. KostenNicotine Transdermal Patch and Atypical Antipsychotic Medications for Smoking Cessation in Schizophrenia am J Psychiatry, November 1, 2000; 157(11): 1835 – 1842.[Abstract] [Full Text] C. Kelly and R. McCreadieCigarette smoking and schizophrenia Adv. Psychiatr. Treat., September 1, 2000; 6(5): 327 – 331.[Full Text] A. E. EVINS and T. TISDALEBupropion and Smoking Cessation am J Psychiatry, may 1, 1999; 156(5): 798a – 799.[Full Text] J. AddingtonGroup Treatment for Smoking Cessation Among Persons with Schizophrenia Psychiatr Serv, July 1, 1998; 49(7): 925 – 928. [Abstract] [Full Text] [PDF] Abstract Full Text (PDF) Alert me when this article is cited Alert me if a correction is posted Citation Map Email this article to a Colleague Similar articles in this journal Similar articles in PubMed Alert me to new issues of the journal Add to my Articles & Searches Download to citation manager Citing Articles via HighWire Citing Articles via Google Scholar Articles by Addington, J. Articles by Addington, D. Search for Related Content PubMed Citation Articles by Addington, J. Articles by Addington, D.
Get information about faster international access.
Copyright 1998 American Psychiatric Association. All rights reserved.
Home | Search | Current Issue | Past Issues | Subscribe | All APPI Journals | Help | Contact us