Antibiotic-Associated Colitis is a medical condition, in which large intestine’s inflammation caused by using antibiotics, occurs.
Various antibiotics alter the balance among the bacteria’s quantity and types in the intestine, allowing specific disease causing bacteria to multiply. the bacterium called Clostridium Difficile most commonly results in problems; it produces 2 toxins that may injure the large intestine’s protective lining. the antibiotics that most frequently result in Antibiotic-Associated Colitis include Cephalosporins (for example, Cephalothin), Ampicillin, and Clindamycin. Other antibiotics may include Tetracycline, Penicilines, Chloramphenicol, Trimethoprim-Sulfamethoxazole, and Erythromycin.
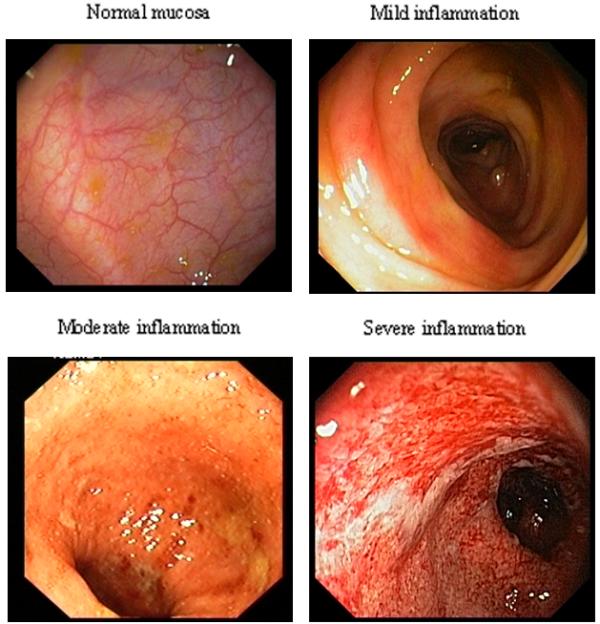
Overgrowth of Clostridium Difficile may happen whether such antibiotic are used by injection or taken by mouth. the risk of having Antibiotic-Associated Colitis increases with age, although, children and young adults may be affected. In mild cases of the disease, the intestine’s lining can become slightly inflamed. In severe cases, an inflammation is extensive and the intestine’s lining is ulcerative.
The symptoms of Antibiotic-Associated Colitis starts while an individual takes the antibiotic. however, in 1/3 of the people, symptoms do not occur until one to ten days after treatment is discontinued, and in some patients, symptoms do not occur as long as six weeks after treatment with antibiotics has stopped. Usually, the symptoms range from mild to bloody diarrhea, fever, and abdominal ache. In some cases, severe dehydration, small intestine perforation, toxic megacolon, and low blood pressure occurs.
Diagnosis of Antibiotic-Associated Colitis is made by examining the large inflamed intestine by using Sigmoidoscope. A Colonoscope can be used if the Sigmoidoscope can not reach higher diseased intestine’s part. Antibiotic-Associated Colitis diagnosis is confirmed, when bacterium Clostridium Difficile is found by performing a test from patient’s stool sample culture or if its toxin is found in the stool. the toxin may be identified in 20% of people with Antibiotic-Associated Colitis and in about 90% of people with severe colitis. during severe attacks, laboratory tests can detect abnormally large count of white blood cells.
Antibiotic-caused diarrhea often relieves within ten to twelve days after antibiotic has been discontinued. In this situation, no other therapy is needed, but if mild symptoms persist, a drug Cholestyramine can be helpful, possibly because it binds itself to the toxins. for severe cases of Antibiotic-Associated Colitis, the antibiotic called Metronidazole is considered to be effective against bacterium Clostridium Difficile. the antibiotic Vancomycin is used for most resistant and severe colitis.
this entry was posted on Thursday, April 7th, 2011 at 1:04 am and is filed under Diseases and Conditions.
Tags: colitis, disease causing bacteria, large intestine, small intestine
You can follow any responses to this entry through the RSS 2.0 feed. You can leave a response, or trackback from your own site.