 The new genetic approach could make the PSA screening test for prostate cancer more accurate. (CBC)
The new genetic approach could make the PSA screening test for prostate cancer more accurate. (CBC)
Scientists have taken a first step toward improving problematic PSA tests for prostate cancer, by mixing in some genetic information that might help tell which men really need a biopsy.
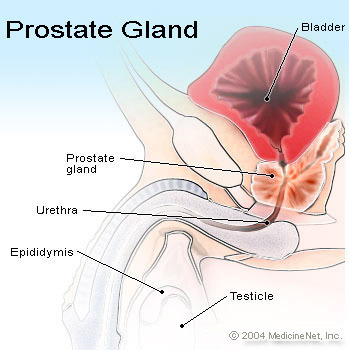
The widely used blood tests measure a protein named PSA that only sometimes signals prostate cancer is brewing. a patient’s PSA level can be high for other reasons, but doctors order a biopsy to check for a tumour whenever PSA reaches a certain level.
Now scientists have discovered a set of genetic variants that show those cutoffs may be skewed for some men because their normal PSA level is naturally much higher than the average that PSA testing was based on.
That means “you end up biopsying a lot of prostates that did not need any biopsy,” said Dr. Kari Stefansson, chief executive officer of deCODE Genetics in Iceland.
His team reported the findings Wednesday in the journal Science Translational Medicine.
Stefansson said he plans to develop a test for those genetic markers, perhaps later next year, in hopes that doctors could use the information to customize how they read and react to their patient’s PSA test results.
This genetic approach makes sense but “I don’t think that this test is ready for prime time” without more research to confirm the findings, cautioned Dr. Otis Brawley, chief medical officer of the American Cancer Society, who wasn’t part of the study.
“It’s important, but it’s a small step in the long road ahead” for better prostate cancer detection, he said.
Finding deadly cancers
Making a PSA test more accurate solves only part of the problem, Brawley stressed. Screening often detects small prostate tumors that will prove too slow-growing to be deadly, but there’s no sure way to tell in advance who needs aggressive therapy.
“What we desperately need is some type of test … that tells us, this is the kind of prostate cancer that kills versus the kind of cancer that doesn’t kill,” he said.
More than 190,000 cases of prostate cancer will be diagnosed this year in U.S. men, and it will kill about 27,000. but routine screening is highly controversial: while most men over 50 have had at least one PSA test, many major medical groups don’t recommend them over fears they may do more harm than good.
The cancer society, for instance, advises that men be told of the pros and cons of the test and decide for themselves.
Among the problems: more than a third of men with PSA levels of 10 or more have no evidence of prostate cancer at biopsy, and many doctors order a tumour check at levels lower than that, around four. Conversely, some men with very low PSA levels wind up with cancer.
Stefansson’s team discovered a set of genetic variants that alters how much PSA, or prostate specific antigen, men naturally produce.
The team reported that men who bear any of three of those variants had PSA levels about 40 per cent higher than average men. When they examined the records of nearly 4,000 men in Iceland and Britain who underwent prostate biopsies, those high-PSA producers were more likely to have had an unnecessary biopsy.
Conversely, men with a fourth variant had PSA levels about 40 per cent lower than average.
Roughly five per cent of men fall into each category, Stefansson said.
What does that mean? if a doctor usually orders a biopsy for a PSA of four, a high-PSA producer might not need one until reaching almost six, Stefansson said. but a low-PSA producer might need one sooner.
The Canadian Cancer Society suggests men over 50 should talk to their doctor about getting tested for prostate cancer. it also suggests that if you are over 40 and have a higher risk of developing the disease, you should talk to your doctor about getting tested.
But for healthy men with no symptoms of the disease, the Canadian society notes there are no recommended screening tests.