 November 2, 2010 in Features Maura Lerner Minneapolis Star Tribune
November 2, 2010 in Features Maura Lerner Minneapolis Star Tribune
- Tweet
- Share
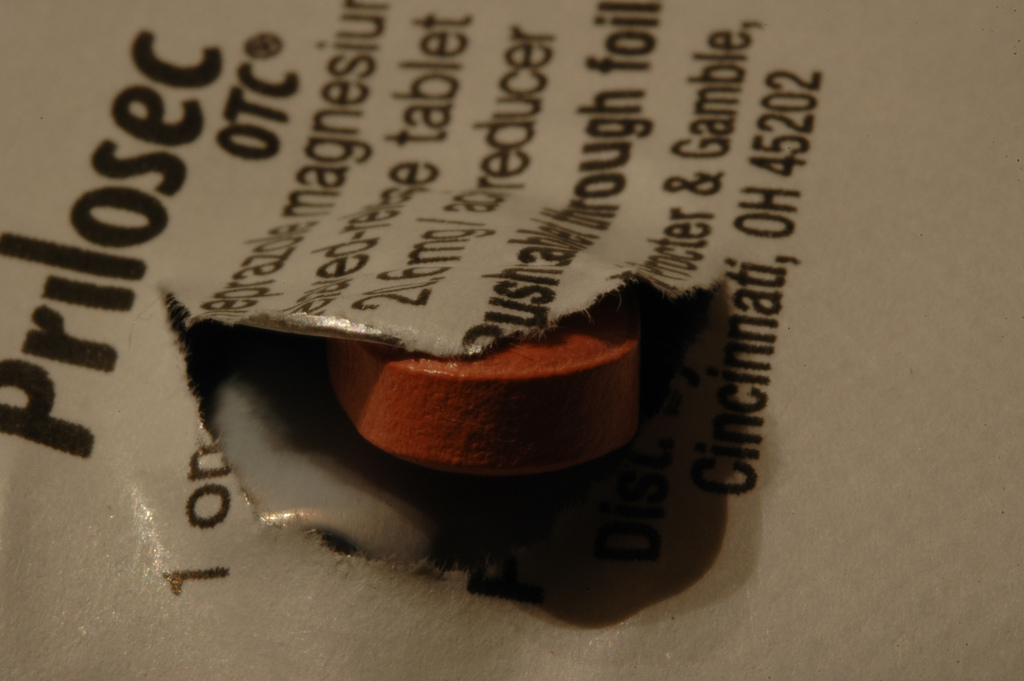
Dr. Marcus Thygeson once wrote his patients countless prescriptions for heartburn drugs such as Prevacid, Prilosec and Nexium – the “little purple pills” of TV ads.
But several months ago, when his own doctor advised him to start taking the pills, he refused.
“It was all I could do to get out of the office without a prescription,” Thygeson says.
The Twin Cities gastroenterologist has come to see the popular pills as a symbol of the excesses of modern medicine – a powerful medication “handed out like water,” in his words, amid mounting evidence that it may do many people more harm than good.
“It’s a drug we’ve become very cavalier about,” says Thygeson, president of the Center for Healthcare Innovation at Allina Hospitals & Clinics. “Now it’s like frontline therapy if you so much as belch.”
The heartburn drugs, known as proton-pump inhibitors (PPIs), are designed to reduce the body’s ability to pump acid into the stomach.
Today, they are among the nation’s best-selling medications, with more than 119 million prescriptions written last year, in addition to over-the-counter sales.
Experts have called them a godsend for ailments like acid reflux, a major cause of heartburn.
Yet there’s a growing consensus that millions of people are taking the pills needlessly, or far longer than necessary, wasting billions of dollars – and, in some cases, triggering significant side effects.
Some skeptics even dare to ask why so many Americans are taking pills, which can cost up to $200 a month, to control digestive problems that can be tied to their own bad habits, particularly at the dinner table.
“I’m not blaming patients – it’s the path of least resistance,” says Dr. Greg Plotnikoff, an internist at Abbott Northwestern’s Penny George Institute for Health and Healing in Minneapolis.
Fixing the underlying problem, he says, may require losing weight, avoiding certain foods or other lifestyle changes. A pill can seem like an easy alternative.
“When I was a resident, I was told it was a quick and easy answer to everything, and it had no side effects, and insurance was willing to pay for it,” Plotnikoff says.
In the past few years, though, scientists have raised concerns about long-term side effects, such as bone fractures and pneumonia.
One study in 2009 even found that the drugs, when stopped abruptly, can cause the very symptoms they were designed to prevent.
The drug manufacturers and some leading experts have disputed those findings. But insurers and doctors alike are starting to have second thoughts.
“When you put a patient on a PPI, you’re essentially setting them up to be on it for a lifetime,” says Thygeson. “I think we need to back away from those drugs.”
Long-term relationships
Bernice Koniar had every reason to feel grateful when her doctor started her on heartburn medication.
The Minnetonka, Minn., woman had just learned she had gastroesophageal reflux disease (GERD), a cause of chronic acid indigestion and all-around misery. and there was nothing more effective for that condition, experts said, than this new class of acid-suppressing drugs.
Actually, they were the second big breakthrough. the first, cimetidine (Tagamet), revolutionized treatment by blocking acid production for short periods.
Then Prilosec, the first proton-pump inhibitor, made its debut in 1989.
“This drug was a miracle,” says Dr. Robert Ganz, a Twin Cities gastroenterologist.
It was remarkably effective for GERD, a condition that causes stomach acid to leak into the esophagus, which in turn can cause burning sensations, nausea and even permanent damage.
In the past, Ganz says, doctors could offer little beyond temporary relief (Tums or Mylanta) or, for severe cases, surgery.
“Without this drug, you’d have 20 million people going to surgery,” he says. “This drug was one of the great pharmaceutical discoveries … of all time.”
It’s now a certified blockbuster, with $13.6 billion in sales last year (more, counting over-the-counter sales).
Prilosec was approved for “short-term treatment (four to eight weeks)” for most symptoms, according to its label.
AstraZeneca, which makes Prilosec and Nexium, said its own studies showed that nine-tenths of acid reflux patients “successfully healed” in eight weeks.
But once the Food and Drug Administration gave its blessing, doctors were free to prescribe them for as long as they liked.
As a result, patients like Koniar have been taking the pills for years. Now 66, she weaned herself off the medication about a month ago.
“I was just taking a drug for something that didn’t exist anymore,” she says.
Pill-pushing popularity
In recent years, several studies have suggested that many people are taking the drug for no apparent reason.
In one Michigan hospital, researchers reviewed patient charts in 2005 and concluded that 60 percent were started on acid-suppressing drugs with no valid explanation.
In May, an editorial in the Archives of Internal Medicine claimed that 53 to 69 percent of the prescriptions for acid suppressors are “for inappropriate indications.”
Dr. David Peura, an industry consultant and former president of the American Gastroenterological Association, readily admits that the drugs are overused.
But he says that’s partly because doctors are reluctant to take patients off medicine if it seems to be working.
“One of the first rules in medicine is, don’t poke a skunk,” says Peura, a retired academic and researcher in Virginia. “That’s why I think a lot of people are probably on the medicine who probably don’t need it.”
At the same time, he and others say, the reasons for using the drugs have expanded.
They’re widely used to prevent ulcers in vulnerable patients, such as the elderly who take daily aspirin. some doctors even use them to diagnose patients with vague symptoms.
Instead of ordering a diagnostic procedure, such as an endoscopy, they might give the patient the drug to see if they improve, says Ganz, a partner in Minnesota Gastroenterology.
“What’s the downside?” he asks. “I might make you feel better. I’m saving you an invasive test.”
And if it works, he says, “I’m a hero.”
Critics, though, aren’t so sure. In the past few years, studies have linked the drugs to an increased risk of bone fractures, pneumonia and an intestinal infection called C. difficile.
There’s also concern the medication may interfere with a heart drug, Plavix.
And last year, researchers in Denmark found that healthy volunteers who took the drugs for eight weeks experienced heartburn and other symptoms when they abruptly stopped.
It’s what scientists call the “rebound effect.” the theory is that when someone stops taking the drug, the acid production system kicks into overdrive, causing even harsher symptoms.
“It’s the best business model ever,” says Plotnikoff, a longtime critic. “The more you take it, the more you need it.”
His solution: Wean patients slowly.
Industry scientists, as well as some national experts, downplay concerns about the rebound effect and say the studies on bone fractures and other side effects are flawed and inconclusive.
“The concern about acid rebound is really not a significant concern,” says Dr. David Johnson, chief of gastroenterology at Eastern Virginia Medical School and a consultant to drug manufacturers.
If symptoms recur, he says, it’s probably due to the underlying condition.
Johnson also says the evidence of side effects is weak and contradictory. his own review, published in April, found no evidence that the drugs interfere with Plavix, for example.
AstraZeneca, one of the largest manufacturers, did not respond to requests for comment.
However, an official at Takeda Pharmaceuticals, which makes Prevacid and Dexilant, says the company takes the concerns seriously.
“The data are far from clear,” says medical director Dr. Gilles Delecoeuillerie. As a result, the company is conducting its own tests on the reported side effects.
But concerns about overuse and safety are starting to change attitudes, even if the risks are low, says Peura, who has studied the drugs extensively.
“The paradigm has sort of shifted,” he says. “We recognize that we should probably be taking people off the medication, or at least lowering the dose.”
But as someone who’s been taking the pills himself for years, Peura knows that may not be easy.
“They made people really feel good for the first time,” he says.
And doctors are under more pressure than ever to find a quick fix for patient complaints.
“If we can deal with that with a pill,” Peura says, “we’ll do it.”