 Hot Flashes Symptoms
Hot Flashes Symptoms
Hot flashes feel as a sudden wave of mild or intense body heat caused by rushes of hormonal changes resulting from decreased levels of estrogen in female body. they are due to blood vessel opening and constricting and a symptom of menopause.
Hot flashes are episodes that are experienced by many, but not all, women undergoing menopause. a hot flash is a feeling of warmth, sometimes associated with flushing that spreads over the body and sometimes followed by perspiration. Menstruating women in their 40′s may have hot flashes, and hot flashes may last for a decade or more in some women. there is no way to predict when they will cease in a given woman. they decrease in frequency over time.
During a hot flash, sensations of heat move up your waist, chest, neck, and face. Perspiration that you exude during your hot flash will soon cool you down, causing you to experience rapid chills all over your body. Typically, a hot flash last only a couple of minutes, however, some unfortunate women can experience hot flashes lasting up to 30 minutes. Women can experience as many as 15 hot flashes in one day, but typically hot flashes occur 2 to 4 hours apart during menopause.
When you’re having a hot flash, you may experience:
- A feeling of pressure in your head as the hot flash begins
- A feeling of mild warmth to intense heat spreading through your upper body and face
- A flushed appearance with red, blotchy skin on your face, neck and upper chest
- Rapid heartbeat
- Perspiration, mostly on your upper body
- A chilled feeling as the hot flash subsides
Less common symptoms associated with hot flashes include:
- Weakness
- Fatigue
- Faintness
- Dizziness
Reasons for Hot Flashes
Exact cause of hot flashes isn’t known, but the signs and symptoms point to factors affecting the function of your body’s thermostat — the hypothalamus. This area at the base of your brain regulates body temperature and other basic processes. The estrogen reduction you experience during menopause may disrupt hypothalamic function, leading to hot flashes. So, hot flashes may have more to do with fluctuation of hormone levels as opposed to low hormone levels per se.
Low estrogen alone doesn’t often seem to induce hot flashes, as children and women with low levels of estrogen due to medical conditions usually don’t experience hot flashes. instead, the withdrawal of estrogen, as happens during menopause, appears to be the trigger.
As estrogen and progesterone levels drop during menopause, the body produces more of a brain hormone called gonadotropin hormone (GnRH) in order to force fertility. GnRH is also responsible for regulating heat sensors in the brain. when higher levels of GnRH are present, the body mistakenly thinks that it is overheating. it attempts to cool itself down by opening blood vessels in the head and neck, which causes perspiration.
Sweaty Side Effects
The most obvious side effect of hot flashes is the sweating! The amount of sweat that your body produces during a hot flash will vary depending on your stage of menopause, your diet, and any medications that you are taking. Some women get away with just a sweaty lip while others feel like they’ve run 10 miles in a fur coat! if your transition between perimenopause and menopause is fairly quick, you can probably expect your symptoms to be a little worse.
Hot flashes can cause you to feel more than just sticky though. It’s not unusual to feel completely exhausted, as though all your energy has been zapped for as much as an hour after a hot flash. On top of that, hot flashes often occur at night, making it impossible to get a good night’s sleep.
Hot flashes leave a lot of women feeling very anxious because they are hard to predict. though you may feel embarrassed if you have a hot sweat at a restaurant, at a friend’s house, or during that big board meeting, remember: most women will go through this at some stage in their life. No one will judge you over a little sweat.
Risk Factors
Not all women who go through menopause experience hot flashes. Although it’s not clear why some women get hot flashes and others don’t, the following factors increase your risk of hot flashes:
- Smoking. Women who smoke are more likely to get hot flashes.
- Obesity. a high body mass index (BMI) is associated with a higher frequency of hot flashes.
- Physical inactivity. if you don’t exercise, you’re more likely to have hot flashes during menopause.
- Ethnicity. More African-American women report menopausal hot flashes than do women of European descent. Hot flashes are less common in women of Japanese and Chinese descent than in white European women.
Lifestyle Tips
Here are some tips to help dealing with hot flashes:
- Know your triggers. keep a daily record of your hot sweats, including how long they last and when they occur. certain foods often exacerbate hot sweats especially spicy foods, hot drinks, and alcohol.
- Keep cool. Slight increases in your body’s core temperature can trigger hot flashes. Dress in layers so that you can remove outer clothing when you feel too warm. Open a window or use a fan or air conditioner to keep air flowing. lower the room temperature, if you can. if you feel a hot flash coming on, sip a cold drink. Avoid hot baths, spring showers and steam baths, esp. before bedtime. Have cool showers, instead.
- Use cotton bed linens. Cotton is more breathable and absorbent than other fabrics. it will keep you cooler at night and help you get a great rest.
- Watch your diet. Drink lots of water and juice and keep a cool drink by your bed. many foods are thought to contribute to or worsen discomfort from hot flashes. Alcohol, caffeine, excess sugar, dairy products, meat products and spicy foods rank among the top aggravators of severe hot flashes as well as mood swings.
- Relax! Learn yoga, listen to music, or engage in quiet meditation.
- Breathe deeply. Deep, slow abdominal breathing (paced respiration) may decrease hot flashes. it takes some practice to perfect the technique, but paced respiration done for 15 minutes twice daily, or at the beginning of a hot flash, can be helpful. To practice paced respiration, begin by sitting comfortably. Breathe in deeply for five seconds, pushing your stomach muscles out. Exhale for five seconds, pulling your stomach muscles in and up. Repeat this cycle of breathing deeply in and out until you feel calm and relaxed.
- Stop smoking. Smoking is linked to increased hot flashes. by not smoking, you may reduce hot flashes, as well as your risk of many serious health conditions such as heart disease, stroke and cancer.
Medications
Menopause is a natural transition. if hot flashes don’t interfere with your life, you don’t need treatment. if it’s necessary to ease your symptoms with treatment, periodically re-evaluate your need for continuing that treatment. for most women, hot flashes fade gradually within a few years.
Hormone therapy
For moderate to severe hot flashes, your doctor may recommend hormone therapy. Estrogen therapy is the most effective treatment for hot flashes, but in some instances, doctors might prescribe progesterone therapy instead.
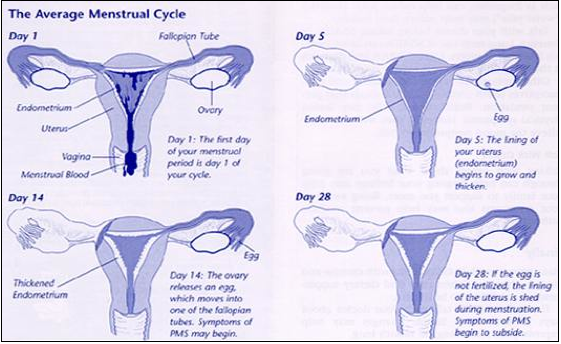
- Estrogen therapy. if you’ve had a hysterectomy, you can take estrogen alone. But if your reproductive organs are still intact, you should take progesterone along with estrogen to protect against cancer of the lining of the uterus (endometrial cancer). With either regimen, current recommendations are to use the lowest effective dose for the shortest amount of time needed to relieve symptoms.
Before starting estrogen therapy for menopause symptoms, review your heart-disease risk factors with your doctor and weigh the benefits of symptom relief against the risk — remote but recognized — of developing heart disease as a result. It’s likely that hormone therapy interacts with other factors — timing and length of hormone use, reproductive history and family history, for example — to increase this risk, but there’s no way to know what’s safest for you individually. Your doctor can help you weigh the pros and cons.
Estrogen therapy is not a good option if you’ve ever had a blood clot or breast cancer.
- Progesterone therapy. As an alternative for women who can’t take estrogen, some doctors prescribe progesterone alone to control hot flashes. Two progesterone-like drugs, megestrol acetate and medroxyprogesterone acetate, have been found to provide some relief from hot flashes.
Other prescription medications
If you decide against estrogen or progesterone therapy, your doctor may suggest a non-hormonal medication for reducing hot flashes. These medications aren’t approved by the Food and Drug Administration specifically to treat hot flashes, but they are approved for treating other conditions.
- Antidepressants. low doses of certain antidepressants may decrease hot flashes. Antidepressants from classes of medications known as selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs) — including venlafaxine (Effexor), paroxetine (Paxil), fluoxetine (Prozac), citalopram (Celexa), desvenlafaxine (Pristiq) and others — have been found to relieve hot flashes. However, these medications aren’t as effective as hormone therapy for severe hot flashes and may cause unwanted side effects, such as nausea, dizziness, weight gain or sexual dysfunction. Talk with your doctor about whether the benefits outweigh the potential side effects for you.
- Gabapentin. Gabapentin (Neurontin) is a medication approved for treating seizures or pain associated with shingles. It’s also increasingly used to treat various other types of pain. Gabapentin may be moderately effective in reducing hot flashes, particularly for women who have symptoms at night. Side effects can include drowsiness, dizziness and headaches.
- Clonidine. Clonidine, a pill or patch typically used to treat high blood pressure, may provide some relief from hot flashes. Side effects such as dizziness, drowsiness, dry mouth and constipation are common, sometimes limiting the medication’s usefulness for treating hot flashes.
Diet, Vitamins, and Natural Remedies
Soy Products
Several researches suggest that soy may have some benefit for reducing hot flashes and other symptoms of menopause. However, it is strongly recommended that you get your soy from foods rather than from supplements. Foods that contain soy include tofu, tempeh, miso, soy milk, whole soybeans, texturized vegetable protein, and soy powder.
Vitamin E
A study published in Gynecologic and Obstetric Investigation found that Vitamin E may help reduce the occurrence and severity of hot flashes and night sweats during menopause. However, a placebo-controlled, randomized study evaluated vitamin E supplements (800 IU/day for four weeks) for 120 breast cancer survivors with hot flashes and found that vitamin E only marginally decreased hot flashes.
Black Cohosh (Actaea racemosa, Cimicifuga racemosa)
This herb has received quite a bit of scientific attention for its possible effects on hot flashes. Studies of its effectiveness in reducing hot flashes have produced mixed results. However, some women report that it has helped them. Recent research suggests that black cohosh does not act like estrogen, as once thought. This reduces concerns about its effect on hormone-sensitive tissue (eg, uterus, breast). Black cohosh has had a good safety record over a number of years. there have been some reports linking black cohosh to liver problems, but this has not been proven.
Red Clover (Trifolium pratense)
In five controlled studies, no consistent or conclusive evidence was found that red clover leaf extract reduces hot flashes. As with black cohosh, however, some women claim that red clover has helped them. Studies report few side effects and no serious health problems with use. But studies in animals have raised concerns that red clover might have harmful effects on hormone-sensitive tissue.
Chasteberry (Vitex agnus castus)
Similar to black cohosh, chasteberry appears to act like a progesterone and has been used in Europe for many years to alleviate PMS symptoms as well as menopausal symptoms. it may help diminish both LH and FSH and appears to affect your pituitary function. Different studies have found that it reduced menopausal symptoms, particularly hot flashes and irregular bleeding. And it appears to be very helpful for breast tenderness, primarily because chasteberry suppresses prolactin production. Typically, it takes about three to four weeks notice results. one note, however: While chasteberry is widely used in Europe, there have been no double-blind placebo studies conducted on it.
Dong Quai (Angelica sinensis)
Dong quai has been used in Traditional Chinese Medicine to treat gynecologic conditions for more than 1,200 years. Yet only one randomized clinical study of dong quai has been conducted to determine its effects on hot flashes, and this botanical therapy was not found to be useful in reducing them. Some experts on Chinese medicine point out that the preparation studied was not the same as they use in practice. Dong quai should never be used by women with fibroids or blood-clotting problems such as hemophilia, or by women taking drugs that affect clotting such as warfarin (Coumadin) as bleeding complications can result.
Ginseng (Panax ginseng or Panax quinquefolius)
Research has shown that ginseng may help with some menopausal symptoms, such as mood symptoms and sleep disturbances, and with one’s overall sense of well-being. However, it has not been found to be helpful for hot flashes.
Kava (Piper methysticum)
Kava may decrease anxiety, but there is no evidence that it decreases hot flashes. it is important to note that kava has been associated with liver disease. The FDA has issued a warning to patients and providers about kava because of its potential to damage the liver.
Evening Primrose Oil (Oenothera biennis)
This botanical is also promoted to relieve hot flashes. However, the only randomized, placebo-controlled study (in only 56 women) found no benefit over placebo (mock medication). Reported side effects include inflammation, problems with blood clotting and the immune system, nausea, and diarrhea. it has been shown to induce seizures in patients diagnosed with schizophrenia who are taking antipsychotic medication. Evening primrose oil should not be used with anticoagulants or phenothiazines (a type of psychotherapeutic agent).
Sources and Additional Information:medterms.com/script/main/art.asp?articlekey=7322epigee.org/menopause/hot_flashes.htmlmayoclinic.com/health/hot-flashes/DS01143/menopause.org/hotflashes.aspxwomenshealth.about.com/cs/hotflashes/a/nomorehotflashs.htm