For the first time, researchers have discovered a disease mechanism that links hereditary amyotrophic lateral sclerosis to the more common “sporadic” form of ALS — and points to a possible therapeutic target.
The findings are reported online in advance of publication in the journal Nature Neuroscience.
ALS is an adult-onset disease that causes progressive degeneration of motor neurons and death within three to five years of diagnosis.
Scott Brady, professor and head of anatomy and cell biology at the University of Illinois at Chicago College of Medicine, studies how neurons shuttle proteins from the cell body, where they are made, down the long “axon” of the nerve cell to the synaptic terminals where they are needed. Disruption of axonal transport is proving to be common factor in a number of adult-onset neurodegenerative diseases, says Scott, who is one of the new study’s authors.
Such disruption results in loss of transmission of signals from one neuron to another, and eventually to a “dying-back” of the axons, which form these connections. this loss of connectivity causes symptoms of ALS long before the neurons actually die, says Gerardo Morfini, assistant professor of anatomy and cell biology at UIC and one of the co-authors.
Previous studies showed that the most common cause of hereditary ALS were mutations in a gene for an enzyme called superoxide dismutase-1, or SOD1. But hereditary ALS accounts for less than 10 percent of ALS cases — and only a quarter of hereditary ALS patients have mutations in SOD1.
Researchers, including scientists from UIC, the University of Massachusetts Medical Center, and four other centers, found that another enzyme in nerve cells, called P38 MAP kinase, which was known to be elevated in ALS, was activated by mutant SOD1. When activated, P38 disrupted the transport of material from the cell body to the axon.
“The big question is what causes the disease in the 90 percent of cases without a genetic component, and why is the disease seen in sporadic cases of ALS almost undistinguishable from the hereditary ALS forms?” said Scott.
In this latest paper, based on evidence that some patients with sporadic, or non-hereditary, ALS had a modified form of SOD1, the researchers created an oxidized form of SOD1 that is partially unfolded, which they were able to show also activated P38 and caused the same disruption in the axon’s transport system.
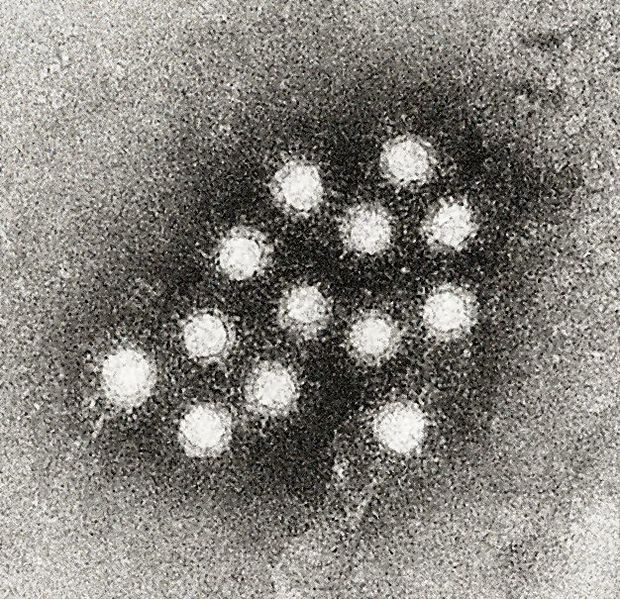
Recently, members of the research team generated a monoclonal antibody to a mutant SOD1 that recognized all of the different mutant forms of SOD1 and yet didn’t react with normal SOD1. it seemed likely, Scott said, that the antibody was reacting with the same key feature that all of the mutants shared. they found that the antibody reacted with oxidized SOD1 as well.
“this told us that you didn’t need a mutation, you just needed a partially denatured protein — a protein that is not quite folded correctly may expose a biologically active domain that activates this pathway,” said Scott.
Team members at the University of Massachusetts Medical Center obtained tissue from the spinal cords of nine patients with sporadic ALS. four of the nine tissue samples from patients — and none of 17 samples from healthy controls — reacted with the antibody, suggesting that misfolded SOD1 was a factor in a significant fraction of patients with sporadic ALS.
“while mutations in SOD1 give rise to only a quarter of hereditary ALS cases, we may be able to relate as much as 50 percent of sporadic ALS to SOD1 misfolding,” said Scott. “this means that if we can find something that can protect patients with the mutation, it should also be able to protect the patients with the misfolded SOD1.”
The new findings identify the specific role of the P38 enzyme in disrupting axonal transport, said Morfini. “this not only defines a therapeutic target, but with a number of p38 inhibitors being investigated, there is real potential that these findings may eventually help patients with ALS.”
Thur work was supported by grants from the National Institutes of Health, the ALS Association, The Angel Fund, ALS Therapy Alliance-CVS Pharmacy, and Project ALS.
Yuyu Song at UIC; Daryl Bosco, Benjamin Fontaine, Nathan Lemay, Diane McKenna-Yasek and Robert H. Brown of the University of Massachusetts Medical Center; N. Murat Karabacak and Jeffrey Agar of Brandeis University; Francois Gros-Louis and Jean-Pierre Julien of Laval University in Quebec; Piera Pasinelli of Thomas Jefferson University in Philadelphia; dvd Holly Goolsby and Mathew Frosch of the C.S. Kubik Laboratory for Neuropathology at Massachusetts General Hospital also contributed to the study.
For more information about UIC, visit uic.edu