The source for this column’s idea actually comes from a parent who, in exasperation, declared that his kids were driving him crazy. He then jokingly asking if there was a vaccine out there that can be used to eliminate Attention Deficit Hyperactivity Disorder (often referred to as ADHD).
Another parent actually had momentary thoughts of selling the kids to the highest bidder and even was willing to go with any bidder at all.
Obviously, these parents were joking as they continue to deal with the stresses of raising kids with ADHD. yet, the comments (despite their attempt at some humor) revealed the depths of distress these parents were experiencing. the problem is not small, either. in 2006, the Centers for Disease Control and Prevention reported that 4.5 million children ages 5 to 17 had been diagnosed with ADHD.
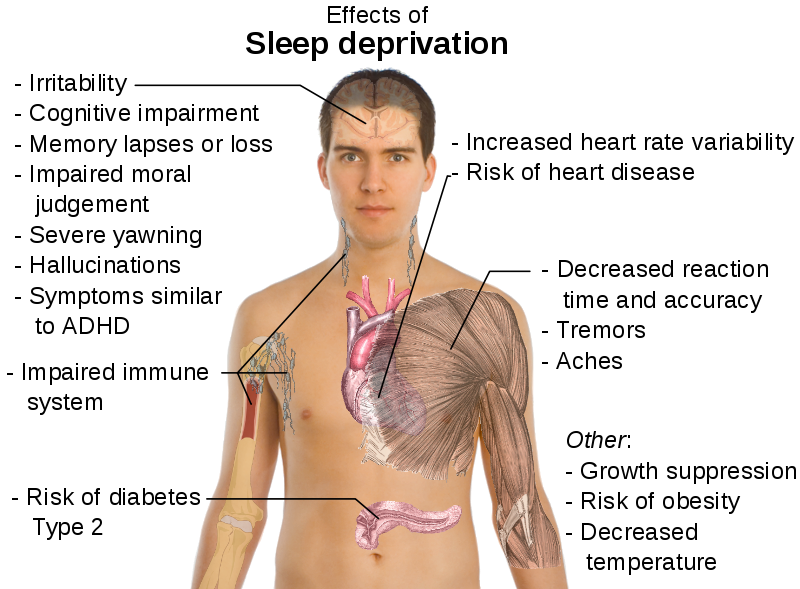
This disorder, in which the main behavioral themes include impatience, impulsivity, inattention to detail, difficulty concentrating and staying focused, forgetfulness, disorganization, being always on the go and so many more annoying traits, can wear out parents, siblings, grandparents and even teachers.
As one author noted, “The brutal reality about children — they’re such powerful stressors that small perforations in relationships can turn into deep fault lines.”
No doubt, the energy of married couples shifts when kids come into the world, and naturally so, but the shift can be disastrous at times. This can be especially true for single parents and even happily married couples when the added stressor is a child with ADHD.
Often the symptoms on first glance at a child’s behavior at home might be viewed by parents as mischievous and may elicit a command from mom or dad “I’m going to count to three” or “OK, you need to go to time-out.”
When school enters the picture, a teacher may begin to notice areas of concern, such as not paying attention, talking, frequent need to be redirected, always seeking attention and coming across as the class clown. Then come the notes from the teacher to mom and dad indicating that Johnny is not turning in homework assignments. the parents discover that what homework Johnny did attempt to complete wasn’t anywhere near what had been assigned. Next is a parent-teacher conference, in which the reality sinks in that the problems at home also are occurring at school.
But there could be an explanation, and referral for a complete assessment by the family physician, pediatrician and/or mental health professional just might reveal that the symptoms and behaviors meet the criteria for considering ADHD. once the diagnosis can be confirmed, medications can do wonders in helping bring about some stability and focus, plus some relief for mom and dad. with good medication management under the supervision of appropriate medical professionals, the light at the end of the tunnel can finally be visible.
The critical pieces include:
n Confirmation of the diagnosis, which then sets a course of action.
n Medication based on a well-developed social/medical history and documentation of symptoms and behaviors.
n Structure, with a routine established even through the summer, so transition from summer break to the rigors of school can be made with minimal stress.
n Constancy, with parents maintaining a routine of communication with the teacher who is in daily contact with the child.
Medications can be a real concern for parents, since stimulants are the most commonly prescribed. the medications in this class of drugs can create a tolerance that sometimes necessitates increasing the dosage, not at all unusual with kids who are in their rapid growth spurt. A visit to the health care professional always includes checking weight and height.
As one author noted, medications often can be a family affair; it’s not at all unusual for more than one person in the home to be on ADHD medicine. This even can include one of the parents.
Such medications are fast-acting, with onset within 30 to 60 minutes, peaking at one to two hours and lasting from two to five hours. Extended release preparations are helpful to reduce the need for school dosing. And, there are longer-acting amphetamines as well.
Sometimes stimulant medications do not work because patients do not tolerate them well. in such cases, there are other medications available. Often, the best source of help for the physician in determining dosing amounts and frequency comes from the person taking the medicine. We always seek our patients’ input on how they think they’re doing; this includes the children. the best source of information on these medications is your family physician, pediatrician, advance practice nurse or psychiatrist.
Don’t give up. with persistence and perseverance, most children will come to grips with the realities of their everyday life and recognize the importance of taking their medications.
Professionals who work with ADHD are available in our communities. Please don’t hesitate to contact someone when help is needed.
Mary Lou Petrisko is a licensed clinical social worker and registered play therapist and Cheryl Thomas is an advanced practice nurse with Mulberry Center Inc. Contact the organization at (812) 436-4221 or comments@south[SR]western.org.