 Wednesday, March 16, 2011
Wednesday, March 16, 2011
The standard retreatment regimen for tuberculosis has low treatment response rates and is associated with poor long term outcomes in certain subgroups of patients, particularly those infected with both HIV and multi-drug resistant TB. these findings from a study by Edward Jones-López from Boston University Medical School, Boston, USA, and colleagues and published in this week's PLoS Medicine, indicate that the standard retreatment approach to TB as implemented in low and middle-income settings, with a high prevalence of HIV, is inadequate and stress the importance of a new, more effective, strategies.
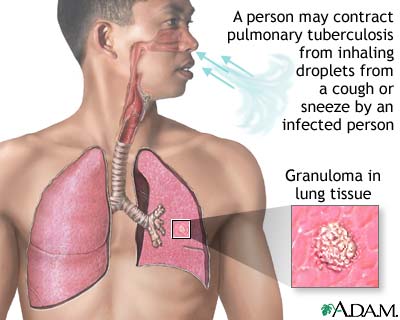
Every year, 10-20% of people with TB in low and middle income countries are started on a standardized five-drug retreatment regimen [(2 SHERZ/ 1 RHEZ/ 5 RHE) meaning 2 months of streptomycin (S), isoniazid (H), ethambutol (E), rifampicin (R) and pyrazinamide (Z); 1 month of R, H, E and Z; and 5 months of R, H and E] as recommended by the WHO. yet, unlike treatment regimens for newly diagnosed TB patients, the recommended retreatment regimen has never been properly evaluated in randomized clinical trials or prospective cohort studies. Rather, this regime was recommended by experts before the current situation of widespread drug-resistant TB arose. Therefore, in this study based in Kampala, Uganda, the authors conducted a prospective cohort study to assess treatment and survival outcomes in patients previously treated for TB and to identify factors associated with poor outcomes.
The authors found that 29/148 (20%) of HIV-uninfected and 37/140 (26%) of HIV-infected patients had an unsuccessful treatment outcome. Factors associated with an unsuccessful treatment outcome were poor adherence, HIV infection, increasing age, and duration of TB symptoms. all patients with multi-drug resistant TB had an unsuccessful treatment outcome.
The authors conclude: “The recommended regimen for retreatment TB in Uganda yields an unacceptable proportion of unsuccessful outcomes. There is a need to evaluate new treatment strategies in these patients.” They add: “clinical trials of new approaches to retreatment TB in areas heavily affected by HIV and TB should be a priority.”
In an accompanying Perspective, Jerome Amir Singh, from the University of Kwazulu-Natal, Durban, South Africa, discusses the ethical context of the Ugandan study. At the time the study was proposed and initiated, the prevalence of multidrug resistant tuberculosis in Uganda was unknown and second-line therapy for this condition, was not locally available leading to two ethical dilemmas — conducting research in a setting where the existing standard of care for the health condition under investigation is “no treatment,” (despite efficacious treatment existing elsewhere) and introducing an efficacious standard of care for a research study in a setting where this standard would not otherwise be available.
After conducting a detailed critique, Dr Singh concludes: “The Uganda study has undoubtedly addressed an important knowledge gap in science. It will hopefully herald revisions to Uganda's TB treatment program and inspire similar reforms elsewhere. Equally significant, the study catalyzed the provision of second-line TB therapy in that country. In so doing, the study has undoubtedly left the local population better off compared to before its commencement. these two factors, alone, make the Uganda study ethically defensible.”
Public Library of Science: plos.org