Can endometrial cancer be discovered by just a transvaginal ultrasound?I was diagnosed with endometrial hyperplasia 2 months ago during an ultrasound. My transvaginal ultrasound also showed abnormalities like an enlarged endometrial stripe. I go back on the 14th because the head of radiology requested for me to have another ultrasound to see if the stripe was still enlarged, the results my primary care physician showed me also said that cancer cannot be ruled out in the patient (me) due to age. (I’m only 22).
Answer by lovelyxxEndometrial cancerFrom MayoClinic.comSpecial to CNN.com
Endometrial cancer is one of the most common cancers in American women. in fact, about 40,000 American women receive a diagnosis of endometrial cancer each year, making it the fourth most common cancer found in women — after breast cancer, lung cancer and colon cancer.
Endometrial cancer usually begins in the lining of the uterus (endometrium). The uterus is a hollow, pear-shaped pelvic organ. Endometrial cancer most often occurs after the reproductive years, between the ages of 60 and 70. Endometrial cancer is sometimes called uterine cancer, but there are other cells in the uterus that can become cancerous — such as muscle or myometrial cells. These form much less common cancers called sarcomas and account for less than 5 percent of uterine cancers.
Endometrial cancer is often detected at an early stage because it frequently produces vaginal bleeding between menstrual periods or after menopause. If discovered early, this slow-growing cancer is likely to be confined to the uterus. Removing the uterus surgically often eliminates the cancer. in fact, stage I endometrial cancer is successfully treated more than 90 percent of the time. Unfortunately, not everyone can be successfully treated because the cancer may have spread beyond the uterus at the time of diagnosis. About 7,000 American women die each year of endometrial cancer.
Endometrial cancer often develops over a period of years. your first clue that something is wrong may be vaginal bleeding that’s uncommon for you.
Most cases of endometrial cancer develop in postmenopausal women, whose periods have stopped. However, a small percentage of cases affects women younger than 40. Signs and symptoms may include:
Prolonged periods or bleeding between periodsMore frequent vaginal bleeding or spotting during the years leading up to menopause (perimenopause)Any bleeding after the time of menopauseA pink, watery or white discharge from your vaginaPelvic pain, especially late in the diseasePain during intercourseWeight lossSometimes, but rarely, endometrial cancers can reach an advanced stage before signs and symptoms are present.
Healthy cells grow and divide in an orderly way to keep your body functioning normally. But sometimes this growth gets out of control — cells continue dividing even when new cells aren’t needed and create cancer.
In endometrial cancer, cancer cells develop in the lining of the uterus. Why these cancer cells develop isn’t entirely known. However, scientists believe that estrogen levels play a role in the development of endometrial cancer. Factors that can increase the levels of this hormone and other risk factors for the disease have been identified and continue to emerge. in addition, ongoing research is devoted to studying changes in certain genes that may cause the cells in the endometrium to become cancerous.
The female reproductive system consists of two ovaries, two fallopian tubes, a uterus and a vagina. The ovaries produce two main female hormones — estrogen and progesterone. The balance between these two hormones changes each month, helping the endometrium thicken in case pregnancy occurs or shed tissue if it doesn’t.
When the balance of these two hormones shifts toward more estrogen — which stimulates growth of the endometrium — a woman’s risk of developing endometrial cancer increases. Factors that increase levels of estrogen in the body include:
Many years of menstruation. If you started menstruating at an early age — before age 12 — and continue to have monthly periods into your 50s, you’re at greater risk of endometrial cancer than is a woman who menstruated for fewer years. The more years you have had a monthly period, the more exposure your endometrium has had to estrogen.never having been pregnant. The body produces more progesterone during a pregnancy, helping protect you from endometrial cancer by lowering levels of estrogen. If you’ve never been pregnant, you don’t get the benefit of this protection.Irregular ovulation. Ovulation, the monthly release of an egg from an ovary in menstruating women, is regulated by estrogen. Irregular ovulation or failure to ovulate can increase your lifetime exposure to estrogen. Ovulation irregularities have many causes, including obesity and a condition known as polycystic ovary syndrome (PCOS). This is a condition in which hormonal imbalances prevent ovulation and menstruation. Treating obesity and PCOS can help restore your monthly ovulation and menstruation cycle, decreasing your risk of endometrial cancer.Obesity. Ovaries aren’t the only source of estrogen. Fat tissue can change some hormones into estrogen. being obese can increase levels of estrogen in your body, putting you at a higher risk of endometrial cancer and other cancers. a high-fat diet also can add to your risk by promoting obesity. Some scientists even think that fatty foods may directly affect estrogen metabolism, further increasing a woman’s risk of endometrial cancer.Diabetes. This is a risk factor for endometrial cancer mainly because obesity and type 2 diabetes often go hand in hand. However, some data suggest that women who have diabetes, whether they’re obese or not, are at greater risk of endometrial cancer.Estrogen-only replacement therapy (ERT). Estrogen stimulates growth of the endometrium. Replacing estrogen alone after menopause may increase your risk of endometrial cancer. taking synthetic progestin, a form of the hormone progesterone, with estrogen — combination hormone replacement therapy — causes the lining of the uterus to shed and actually lowers your risk of endometrial cancer. However, this combination may cause other health risks.Ovarian tumors. Some tumors of the ovaries may themselves be a source of estrogen, increasing estrogen levels.
Other factors that can increase your risk of endometrial cancer include:
Age. most endometrial cancers develop over many years. Therefore, the older you are, the greater your risk. Ninety-five percent of endometrial cancer occurs in women older than 40.Personal history of breast cancer or ovarian cancer. Some of the same risk factors for breast cancer and ovarian cancer also increase your risk of endometrial cancer.Tamoxifen treatment. One in every 500 women whose breast cancer was treated with tamoxifen will also develop endometrial cancer. The drug acts like estrogen in some parts of the body, causing the uterine lining to grow. If you’re being treated with this hormone, see your doctor for an annual pelvic examination and be sure to report any unusual vaginal bleeding.race. White women are more likely to develop endometrial cancer, but black women are much more likely to die of the disease.Hereditary nonpolyposis colorectal cancer (HNPCC). This inherited disease is caused by an abnormality in a gene important for DNA repair. Women with HNPCC also have a significantly higher risk of endometrial cancer.having risk factors for endometrial cancer doesn’t mean you’ll get the disease. it means that you’re at risk and should be alert to possible signs and symptoms of the disease. Conversely, some women who develop endometrial cancer appear to have no risk factors for the disease.
When to seek medical advice
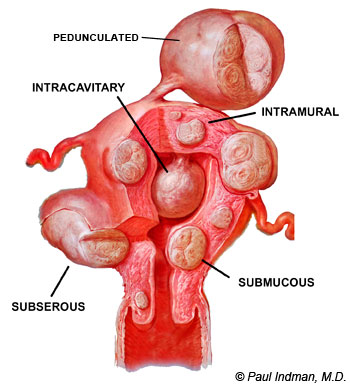
Because endometrial cancer is more likely to be successfully treated the earlier it’s diagnosed, see your doctor if you experience any signs or symptoms of the disease — including vaginal bleeding or discharge not related to your periods, pelvic pain or pain during intercourse. many of the symptoms you experience may be associated with noncancerous (benign) conditions, such as vaginal infections, uterine fibroids or uterine polyps. But it’s still important to bring them to the attention of your doctor.
Many endometrial cancers develop from less serious abnormalities of the endometrium that doctors can detect during routine exams and treat before they turn cancerous. That’s one of the reasons why regular gynecologic examinations are important for all adult women. This is especially true for women at high risk of endometrial cancer. If you’ve had endometrial cancer, ask your doctor about regular follow-up exams to check that the cancer hasn’t returned.
Screening and diagnosis
If your doctor suspects endometrial cancer, you may be referred to a gynecologist — a doctor who specializes in conditions affecting the female reproductive system. The gynecologist or your primary care doctor will conduct a complete medical history and perform a physical and pelvic examination. During the pelvic examination, the doctor feels for any lumps or changes in the shape of the uterus that may indicate a problem.
Diagnosis may or may not involve these other tests:
Pap test. your doctor takes a sample of cells from the cervix, the lower, narrower portion of the uterus that opens into your vagina. Doctors use the Pap test to detect another type of cancer — cervical cancer. because endometrial cancer begins inside your uterus, it’s rarely detectable by a Pap test.Endometrial biopsy. to get a sample of cells from inside your uterus, you’ll likely undergo an endometrial biopsy. This involves your doctor removing a small piece of tissue from your uterine lining for laboratory analysis. This may be done in your physician’s office and usually doesn’t require anesthesia.Dilation and curettage (D and C). If enough tissue can’t be obtained during a biopsy or if the biopsy suggests cancer, you’ll likely need to undergo a D and C. in this procedure, which requires you to be in an operating room under anesthesia, tissue is scraped from the lining of your inner uterus and examined under a microscope for cancer cells.Transvaginal ultrasound. your doctor may also recommend a transvaginal ultrasound to help rule out other conditions. in this painless procedure, a wand-like device (transducer) is inserted into your vagina. The transducer uses sound waves to create a video image of your uterus. This test helps your doctor look for abnormalities in your uterine lining.If cancer of the endometrium is found, you’ll likely be referred to a gynecologic oncologist — a doctor who specializes in treating cancers involving the female reproductive system. You’ll need more tests to determine if the cancer has spread to other parts of your body (metastasis). These tests may include a chest X-ray, a computerized tomography (CT) scan and a blood test to measure cancer antigen 125 (CA 125), a substance that’s released in the bloodstream in some endometrial and ovarian cancers.
Once the diagnosis of endometrial cancer is confirmed, your doctor will want to “stage” your cancer. Staging is how doctors try to determine if the cancer has spread outside of the uterus. in endometrial cancer, staging is done through a surgical procedure and is done at the same time as any surgical treatment:
Stage I cancer is found only in your uterus and hasn’t spread at all.Stage II cancer can be found in the body of both your uterus and your cervix. in this stage, cancer is no longer confined to the uterus, but hasn’t spread beyond the pelvic region.Stage III cancer has not involved the rectum and bladder, though pelvic area lymph nodes may be.Stage IV cancer is the most serious and means that the cancer has spread past the pelvic region and can affect the bladder, rectum and many other parts of your body.Fortunately, about 75 percent of endometrial cancers are diagnosed at stage I or II.
When discovered early, endometrial cancer is usually treatable. However, in some women endometrial cancer reaches an advanced stage before diagnosis.
Endometrial cancer can cause pelvic pain and painful urination. as the cancer advances, symptoms may worsen. Treating the cancer can help alleviate the pain.
Women with endometrial cancer tend also to lose blood from vaginal bleeding. Over time, chronic loss of blood can result in anemia — a condition in which the blood is low on red blood cells and oxygen. Anemia causes fatigue and shortness of breath. But anemia can be treated along with your cancer, helping you regain energy.
Finally, endometrial cancer can recur in some women who don’t have their uterus removed during treatment.
Surgery is the most common treatment for endometrial cancer. most doctors recommend either the surgical removal of the uterus alone (hysterectomy) or, more likely, the surgical removal of the uterus, fallopian tubes and ovaries (complete hysterectomy). Lymph nodes in the area should also be removed during surgery along with other tissue samples during the staging operation. Lymph nodes are small, bean-shaped structures found throughout your body that produce and store infection-fighting cells, but may also be invaded by cancer cells.
A hysterectomy is a major operation, and because you can’t get pregnant after your uterus has been removed, it can be a difficult decision for some women. However, surgery is usually the only way to eliminate the cancer or the need for further treatment.
If you have an aggressive form of endometrial cancer or the cancer has spread to other parts of your body, you may need additional treatments. These may include:
Radiation. Radiation therapy is the use of high-dose X-rays to kill cancer cells. If your doctor believes you’re at high risk of cancer recurrence, he or she may suggest that you have radiation therapy after a hysterectomy. your doctor may also recommend radiation therapy if the cancerous tumor is fast growing, invades deeply into the muscle of the uterus or involves blood vessels. Brachytherapy is another form of radiation that involves the internal application of radiation, usually to the inner lining of the vagina. Brachytherapy has significantly fewer side effects than conventional radiation therapy does. However, brachytherapy treats only a small area of the body.Hormone therapy. If the cancer has spread to other parts of your body, synthetic progestin, a form of the hormone progesterone, may stop it from growing. The progestin used in treating endometrial cancer is administered in different doses from the progestin used in hormone replacement therapy for menopausal women. Some different medications may be used as well. Treatment with progestin may be an option for women with early endometrial cancer who want to have children and, therefore, don’t want to have a hysterectomy. However, this approach is not without the risk that the cancer will return. Carefully discuss this treatment with an expert in this field.Chemotherapy. Chemotherapy is the use of drugs to kill cancer cells. in some cases, your doctor may recommend chemotherapy for endometrial cancer. you may receive chemotherapy drugs by pill (orally) or through your veins (intravenously). These drugs enter your bloodstream and then travel through your body, killing cancer cells outside the uterus.each type of treatment for endometrial cancer can have side effects. ask your doctor what side effects you can expect and what can be done to manage them.
If you have late-stage or recurrent endometrial cancer, you may be at decreased odds for successful treatment with standard therapies. you may benefit from participating in clinical trials that provide new experimental treatment options. For more information on clinical trials, contact the National Cancer Institute at (800) 4-CANCER, or (800) 422-6237, or visit its Web site.
After treatment for endometrial cancer, your doctor will likely recommend regular follow-up examinations to check that the cancer hasn’t returned. Checkups may include a physical exam, a pelvic exam, a Pap test, a chest X-ray and laboratory tests.
Although most cases of endometrial cancer aren’t preventable, certain factors can lower your risk of developing the disease. These include:
Taking hormone therapy (HT) with progestin. Estrogen stimulates growth of the endometrium. Replacing estrogen alone after menopause may increase your risk of endometrial cancer. taking synthetic progestin, a form of the hormone progesterone, with estrogen causes the lining of the uterus to shed. This kind of combination hormone therapy lowers your risk. But not all effects of HT are positive. taking HT as a combination therapy can result in serious side effects and health risks. Work with your doctor to evaluate the options and decide what’s best for you.a history of using birth control pills. Use of oral contraceptives can reduce endometrial cancer risk even as long as 10 years after you stop taking them. The risk is lowest in women who take oral contraceptives for many years.Maintaining a healthy weight. Obesity is one of the highest risk factors for the development of endometrial cancer in most women. you can help prevent endometrial cancer by maintaining a healthy weight. Excess fat tissue can increase levels of estrogen in your body, which increases your risk of endometrial cancer. Maintaining a healthy weight as you age lowers your risk of endometrial cancer as well as other diseases.
Eating well, managing stress and exercising are ways to promote your overall health and cope with any form of cancer.
Eating wellGood nutrition is especially important for people undergoing cancer treatment. But eating well can be difficult if your treatment includes chemotherapy or radiation treatment. you may feel nauseated or lose your appetite, and foods may seem tasteless. you may find that the last thing you want to do is plan meals.
Even so, eating well during cancer treatment can help you maintain your stamina and your ability to cope with the side effects of treatments. good nutrition may also help you prevent infections and remain more active.
Remember these strategies for eating well when you don’t feel well:
Eat protein-rich foods. Foods high in protein can help build and repair body tissues. Eggs, yogurt, cottage cheese, peanut butter, beans, poultry and fish are good sources of protein.when you do feel well, make the most of it. Eat as many healthy foods as you can. Prepare meals that you can easily freeze and reheat. also look for frozen dinners and other prepared foods.Pack calories into the foods you eat. For example, spread butter, jam or honey on bread. Sprinkle foods with chopped nuts.Eat smaller amounts of food more frequently. If you can’t face the thought of a large meal, try eating small amounts of food more often. Keep fruits and vegetables handy for snacking.Managing stressMethods for reducing physical tension can help you manage stress. One simple and powerful technique is to simply close your eyes and notice your breathing. Pay attention to each inhalation and exhalation. your breathing will become slower and deeper, promoting relaxation. another technique is to lie down, close your eyes and mentally scan your entire body for any points of tension.
ExercisingActivities such as running and swimming that require repetitive movements can produce a mental state similar to meditation. so can yoga and other stretching exercises.
Your doctor may have more specific suggestions about how to best care for yourself before, during and after treatment for endometrial cancer.
After you receive a diagnosis of endometrial cancer, you may have many questions, fears and concerns. How will the diagnosis impact you, your family, your work and your future? you may worry about tests, treatments, hospital stays and medical bills. Even if a full recovery is likely, you may worry about recurrence of your cancer.
Fortunately, many resources are available to you and your family to help answer questions and provide support. The key is to remember that you don’t have to face your questions or fears alone. here are some strategies and resources that may make dealing with endometrial cancer easier:
Know what to expect. find out everything you can about your cancer — the type, stage, your treatment options and their side effects. It’s important for you to have honest, open discussions with your cancer care team. The more you know, the more active you can be in your own care. in addition to talking with your doctor, look for information in your local library and on the Internet. Staff of the National Cancer Institute will answer questions from the public. you can reach the cancer institute at (800) 4-CANCER, or (800) 422-6237. or contact the American Cancer Society at (800) ACS-2345, or (800) 227-2345.Be proactive. Although you may feel tired and discouraged, don’t let others — including your family and your doctor — make important decisions for you. Take an active role in your treatment. Before starting treatment, you might also want to get a second opinion from a qualified specialist. many insurance companies will pay for a second opinion.Maintain a strong support system. Strong relationships may help you cope with treatment and survive your cancer. Although friends and family can be your best allies, they sometimes may have trouble dealing with your illness. If so, the concern and understanding of a formal support group or other cancer survivors can be especially helpful. ask your doctor to help you get in touch with a support group in your area.
Answer by LissacalTransvaginal ultrasound can be used to measure the endometrial thickness. But, if it is thickened, ultrasound cannot tell us why it is thickened.
The endometrium grows thicker during your cycle, when the uterus is preparing for a pregnancy. If a pregnancy does not occur, the endometrium sheds, and you have your menstrual period. so, in a woman, still having periods, the endometrium will regularly become thickened, and this is normal. a repeat ultrasound, at a different point of your menstrual cycle, such as right after your period, is a good idea.
To diagnosis endometrial cancer, you would need an endometrial biopsy, so cells could be evaluated via a microscope. best wishes….
Know better? Leave your own answer in the comments! Information about multiple myeloma and other plasma cell neoplasms.
Robotic Hysterectomy for Endometrial Cancer
M. Patrick Lowe, MD, renowned robotic surgeon and gynecologic oncologist at Northwestern Memorial Hospital, will demonstrate the use of robotic surgery to treat endometrial cancer. Dr. Lowe, director of the robotics and minimally invasive surgical program for the Division of Gynecologic Oncology at Northwestern University’s Feinberg School of Medicine, was among the early adopters of robotics to treat gynecologic malignancies, citing precision, improved dexterity and superior patient outcomes among the benefits. “Women diagnosed with a gynecologic malignancy want the shortest route leading back to a degree of normalcy post treatment,” says Lowe. “Robotic surgery offers the path of least resistance, combining shorter recovery times with superior outcomes.”
Information about multiple myeloma and other plasma cell neoplasms.
Share and Enjoy:
- Endometrial Cancer Awareness Ribbon Mouse Pad
- My mother has endometrial cancer, what is the average life expectancy of most patients?
- Can you develop Endometrial Cancer randomly?
- Are ultrasounds, transvaginal ultrasounds and x-rays a good source finding ovarian cancer?
- What does the “Grade” refer to in Endometrial cancer?